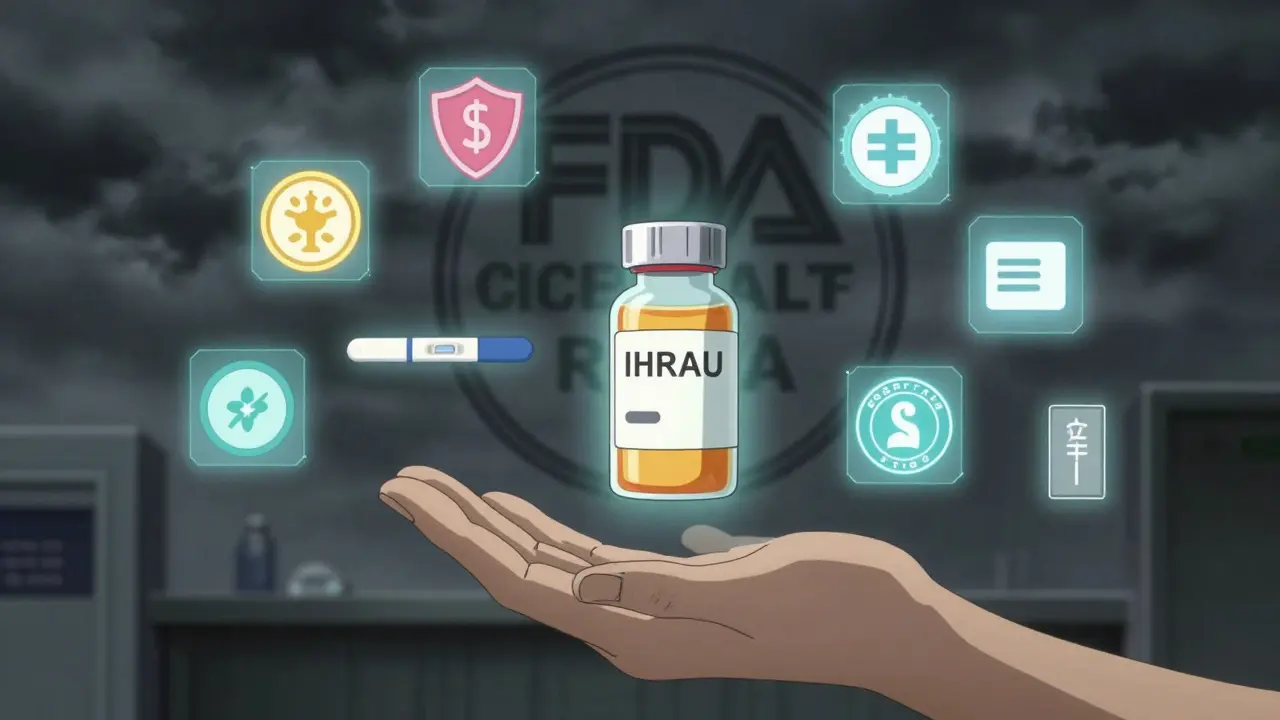
When a drug can save your life but also seriously harm you if used wrong, how do you make sure it’s used safely? That’s the problem the FDA solved with REMS programs - Risk Evaluation and Mitigation Strategies. These aren’t just paperwork. They’re real, enforced systems that control who can prescribe, dispense, and take certain high-risk medications. Without REMS, drugs like thalidomide, clozapine, or lenalidomide might never have made it to patients who need them. But they also create real headaches for doctors, pharmacists, and patients.
What Exactly Is a REMS Program?
A REMS program is a legally required safety plan the U.S. Food and Drug Administration (FDA) forces drugmakers to put in place for medicines with serious, potentially life-threatening side effects. It’s not optional. If the FDA decides the risks of a drug are too high to manage with just a warning label, they demand a REMS. This started in 2007 with the Food and Drug Administration Amendments Act (FDAAA), which gave the FDA clear power to require these programs.
Think of REMS as a safety net. It lets dangerous but necessary drugs stay on the market. For example, isotretinoin (Accutane) can cause severe birth defects. Thalidomide, used for leprosy and some cancers, has the same risk. Without REMS, these drugs would be banned. With REMS, patients can still get them - but only under strict controls.
The Three Core Parts of Every REMS
Not every REMS is the same, but they all include at least one of these three components:
- Medication Guide: A printed handout patients get with their prescription. It explains the biggest risks in plain language. About 78% of REMS programs require this.
- Communication Plan: This targets doctors and pharmacists. It might be a letter, a safety alert, or training materials. About 62% of REMS use this to make sure providers know the risks and how to handle them.
- Elements to Assure Safe Use (ETASU): This is the strictest part. It’s required in about 45% of REMS programs. ETASU can include: prescriber certification, pharmacy certification, restricted distribution to specialty pharmacies, mandatory patient monitoring, pregnancy testing, and even patient enrollment in a registry.
For example, the Revlimid REMS program for lenalidomide - a key drug for multiple myeloma - requires every doctor to be certified, every pharmacy to be registered, every female patient of childbearing age to take monthly pregnancy tests, and every patient to sign a form acknowledging the risks. It’s complex. But without it, the drug couldn’t be legally sold.
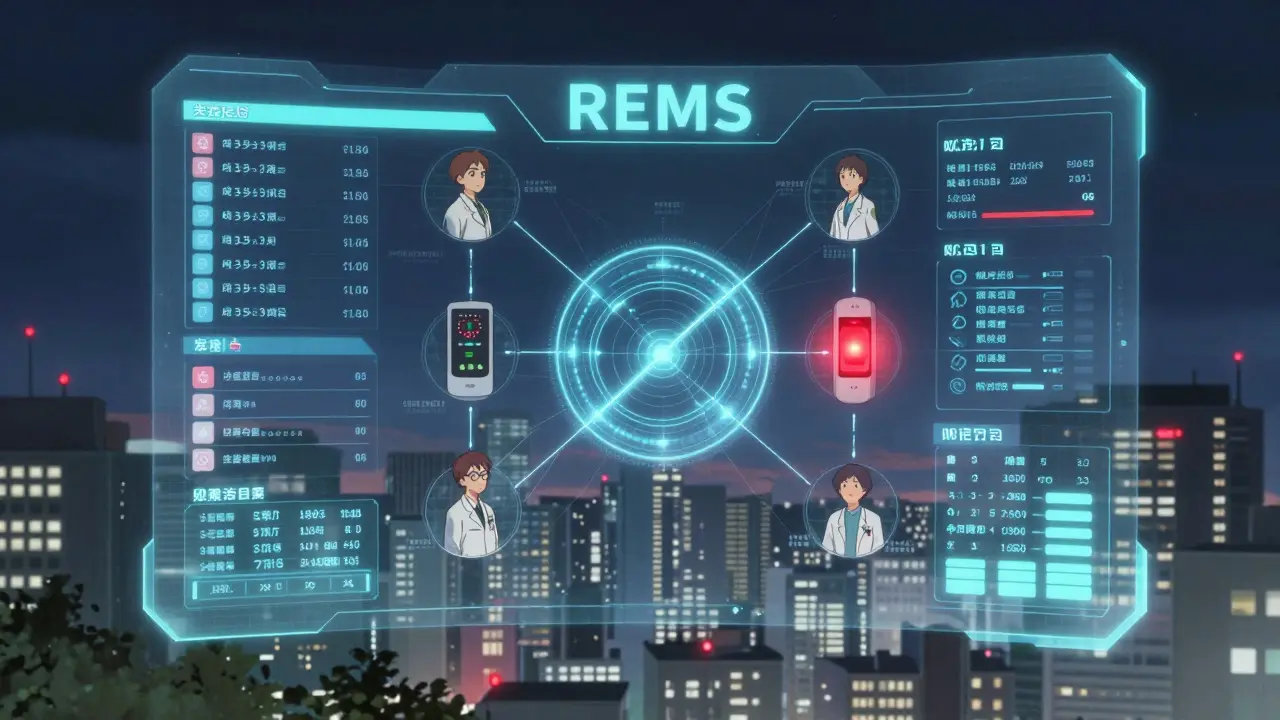
Who Runs REMS Programs?
The drugmaker is legally responsible for designing, funding, and running the REMS. They spend an average of $2.7 million per year on each program. That includes building online portals, training staff, printing materials, and tracking compliance.
But they don’t do it alone. Healthcare providers must complete certification - usually a 45-minute online course - before they can prescribe. Pharmacists must verify that certification before dispensing. Specialty pharmacies handle 89% of REMS drugs because they’re set up to track requirements, store drugs safely, and report data back to the FDA.
Patients are the last link. They have to understand the risks, follow testing schedules, and sometimes travel to specific clinics to get their drug. For drugs like Lemtrada (alemtuzumab), patients must receive the infusion in a hospital under close monitoring - not at a regular pharmacy.

Why REMS Programs Cause Real Problems
REMS saves lives. But they also slow things down - sometimes dangerously.
Doctors spend over five hours a week just managing REMS paperwork for drugs like lenalidomide and pomalidomide, according to a 2023 survey by the American Society of Hematology. Pharmacists say REMS adds 15 to 20 minutes per prescription just to check online portals and print forms. One pharmacist on Reddit wrote: “The Entyvio REMS breaks my workflow. I can’t even fill a prescription without logging into three different systems.”
Patient delays are common. A 2023 GoodRx survey found 42% of patients on REMS drugs experienced treatment delays - sometimes for weeks - because they couldn’t get certified, their pharmacy wasn’t registered, or their pregnancy test wasn’t up to date. For someone with cancer or MS, that delay isn’t just inconvenient. It’s dangerous.
And then there’s the generic drug problem. A 2024 Health Affairs study found that 78% of generic manufacturers said REMS programs delayed their products by an average of 14.3 months. Why? Brand-name companies control the samples needed for testing, and REMS rules make it hard to get them. That keeps prices high and limits access.
How the FDA Keeps REMS in Check
The FDA doesn’t just approve REMS and walk away. They require drugmakers to submit regular reports showing whether the program is working. Are fewer patients having side effects? Are prescribers following the rules? Is the burden too high?
If a REMS isn’t helping, the FDA can remove it. Since 2007, only three REMS programs have been fully discontinued. The most recent was for Zeposia (ozanimod), a multiple sclerosis drug, removed in March 2023 after data showed the risks were manageable with standard labeling.
The FDA also cracks down. In fiscal year 2023, they issued 17 warning letters to drugmakers for REMS violations - a 22% jump from the year before. That means companies are getting sloppy. Maybe they’re not updating training materials. Maybe they’re not tracking patient enrollment. Either way, the FDA is watching.
What’s Changing in 2025 and Beyond
REMS is getting an upgrade. The FDA launched the REMS Modernization Initiative in 2023 to fix the biggest complaints: too much paperwork, too many separate systems, too little transparency.
By Q3 2025, they plan to roll out a public REMS Dashboard - a single website where anyone can see which drugs have REMS, what the requirements are, and how well each program is working. No more hunting through PDFs or calling FDA helplines.
They’re also pushing for electronic systems. Instead of printing forms and faxing certifications, providers will use digital tools that auto-check compliance. The 21st Century Cures Act Reauthorization (2022) demands a new REMS Assessment Standard by December 2025 - a uniform way to measure if a REMS is actually improving safety or just adding red tape.
Experts predict future REMS will use real-world data from electronic health records and wearable devices to monitor patients in real time. Imagine a system that alerts a doctor if a patient on a high-risk drug misses a blood test - before something bad happens.
How Many Drugs Are Covered?
As of November 2024, there are about 120 active REMS programs covering 185 different drugs. That’s roughly 5.7% of all prescription medications in the U.S.
The biggest concentration? Cancer and blood disorders. Hematology/oncology drugs make up 31.7% of all REMS - 38 programs alone. Drugs like Revlimid, Pomalyst, and Thalidomide are all under strict REMS because they can cause birth defects, severe infections, or blood clots.
But it’s not just cancer. REMS also cover drugs for multiple sclerosis (like Lemtrada), severe psoriasis, and rare genetic conditions. The common thread? A high risk that can’t be ignored - but a benefit that’s too important to ban.
The Bottom Line
REMS programs are a necessary evil. They keep dangerous drugs from causing mass harm while still letting patients access life-saving treatments. But they’re broken in places. Too slow. Too confusing. Too expensive.
For patients: If your prescription comes with extra steps - certification, testing, specialty pharmacy - it’s not a mistake. It’s the law. Ask your doctor or pharmacist what you need to do. Don’t skip it.
For providers: Document everything. Use the official portals. Don’t assume your staff knows the rules. Train them. Update your systems.
For the system: Change is coming. The FDA is listening. Digital tools, standardized processes, and better data will make REMS less of a burden - and more of a shield. The goal isn’t to eliminate REMS. It’s to make them smarter.
Are REMS programs only for brand-name drugs?
No. REMS programs apply to both brand-name and generic versions of the same drug. If a brand-name drug has a REMS, the generic version must follow the same rules. Generic manufacturers can’t bypass REMS just because their drug is cheaper. They must comply with the same certification, distribution, and monitoring requirements.
Can a REMS program be removed?
Yes, but it’s rare. The FDA can remove a REMS if evidence shows the program no longer improves safety - or if the risks are now well-managed by standard labeling. Since 2007, only three REMS programs have been fully discontinued. The most recent was for Zeposia in March 2023, after data showed its side effects could be controlled without the extra requirements.
Why do I have to go to a specialty pharmacy for my REMS drug?
Because REMS drugs often need special handling - like cold storage, strict tracking, or mandatory patient counseling. Specialty pharmacies are certified to manage these requirements. Regular pharmacies aren’t trained or equipped to handle the paperwork, certifications, or monitoring. About 89% of REMS programs require distribution through specialty pharmacies to ensure safety.
Do REMS programs actually prevent harm?
Yes. The FDA estimates REMS programs prevent about $8.4 billion in healthcare costs each year by avoiding serious side effects like birth defects, organ failure, or fatal infections. For drugs like thalidomide or clozapine, REMS has prevented thousands of adverse events. The cost of running REMS - $1.2 billion annually - is considered justified by the lives and money saved.
What should I do if my REMS prescription is delayed?
First, contact your prescriber’s office. They may need to re-certify or update your file. Then, call your pharmacy - they might be waiting for a certification check or a patient enrollment form. If it’s been more than a few days, ask for the REMS program’s direct contact number. Most REMS have a support line listed on the FDA’s REMS@FDA website. Don’t wait - delays can be dangerous with high-risk drugs.



Been on a REMS drug for my MS and honestly? The pharmacy staff are saints. They spend 20 minutes just verifying stuff while I sit there wondering if I’ll miss my infusion window. But yeah, I’d rather wait than risk a bad outcome. Worth it.
My dad’s on Revlimid and the whole system feels like navigating a maze blindfolded-but he’s alive because of it. Maybe it’s clunky, but I’d rather have a slow system that works than a fast one that kills people.
REMS is just regulatory capture disguised as patient safety. The brand-name pharma giants use it to block generics by controlling sample access and locking down distribution channels. It’s not about safety-it’s about profit margins. The FDA knows this and still lets it slide.
So let me get this straight-we’re trusting a $2.7M/year corporate program run by the same companies that made the drug to police themselves... and we call this 'safety'? 😂
REMS is just bureaucracy with a heart emoji. It makes everyone feel good while doing nothing real. Patients suffer delays. Providers burn out. And the drug companies? They just raise prices and call it compliance. We’re not protecting lives-we’re protecting balance sheets
As someone who’s worked in oncology pharmacy for 18 years, REMS isn’t perfect-but it’s the best tool we’ve got. I’ve seen patients get thalidomide when they had no other options. The paperwork? Yeah, it’s brutal. But I’d rather fill 50 forms than explain to a family why their baby was born with deformities because we cut corners. The system’s broken, but the intent? Pure.
Have you ever wondered why the FDA only discontinued THREE REMS in 17 years? That’s not because they’re effective-it’s because the FDA is a captive agency, funded and influenced by Big Pharma. They’re not monitoring safety-they’re protecting market exclusivity. The Zeposia removal? A PR stunt. They’ll never touch Revlimid or Lemtrada. Why? Because those are billion-dollar cash cows-and REMS keeps generics off the shelf. You think this is about safety? No. It’s about control.
I love how REMS forces us to think about risk in a way we never did before. It’s not just ‘take the pill’-it’s ‘who are you, what’s your body doing, and how do we make sure you don’t get hurt?’ That’s actually radical. Imagine if every medication came with that level of care. Maybe we’d stop treating people like walking prescriptions and start treating them like humans. The system’s messy, but the philosophy? Kinda beautiful.
In Nigeria, we don’t have REMS programs-yet we have patients on thalidomide and clozapine. No certification. No registry. No specialty pharmacies. Just a doctor’s word and a prayer. I’m not saying our system is better. But I am saying: if a drug is so dangerous that it needs a federal bureaucracy to function, why is it being exported to places without those safeguards? The global inequality in pharmaceutical safety is not an oversight-it’s a design.
It is a matter of national pride and scientific integrity that the United States has implemented such rigorous protocols for the administration of high-risk pharmaceuticals. While other nations may falter in their regulatory oversight, the REMS framework exemplifies the American commitment to patient safety, even at the cost of administrative complexity. This is not red tape; this is responsibility in action.
my dr’s office forgot to re-certify me and i missed 3 weeks of treatment. no one called. no one emailed. just a note in the portal i didn’t check. i’m lucky i didn’t die.
They’re calling it 'REMS Modernization'... but all I see is a bunch of tech bros trying to turn my life-saving meds into a SaaS subscription. Next thing you know, I’ll have to pay $9.99/month to unlock my own blood test reminders. #REMSIsJustUberForCancer
REMS is just the beginning. Soon the FDA will require biometric scans before you can take any drug. They’ll track your sleep, your stress levels, your social media posts-because if you’re depressed, you might forget to take your pill. And if you skip a dose? Your insurance will drop you. This isn’t safety. This is social control dressed in white coats. The government doesn’t want you healthy-they want you compliant.