For years, fish oil supplements have been pushed as a simple, natural way to protect your heart. You’ve seen the ads: take two capsules a day, lower your risk of heart attack, keep your arteries clean. But here’s the truth - the science has changed. A lot. And what worked in 2005 might not work in 2026.
What Exactly Are Omega-3s?
Omega-3 fatty acids are a type of fat your body can’t make on its own. That means you need to get them from food or supplements. The two most important ones for heart health are EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid). These are found mostly in fatty fish like salmon, mackerel, sardines, and herring. Plant sources like flaxseed and chia seeds have a different kind called ALA, but your body turns very little of that into EPA or DHA - so it’s not a reliable substitute.
These fats don’t just float around in your blood. They go to work. They reduce inflammation, help lower triglycerides (a type of fat in your blood), and may stabilize your heart rhythm so it doesn’t suddenly go haywire. That’s why they’ve been tied to heart protection for decades.
The Big Divide: Studies That Agree and Those That Don’t
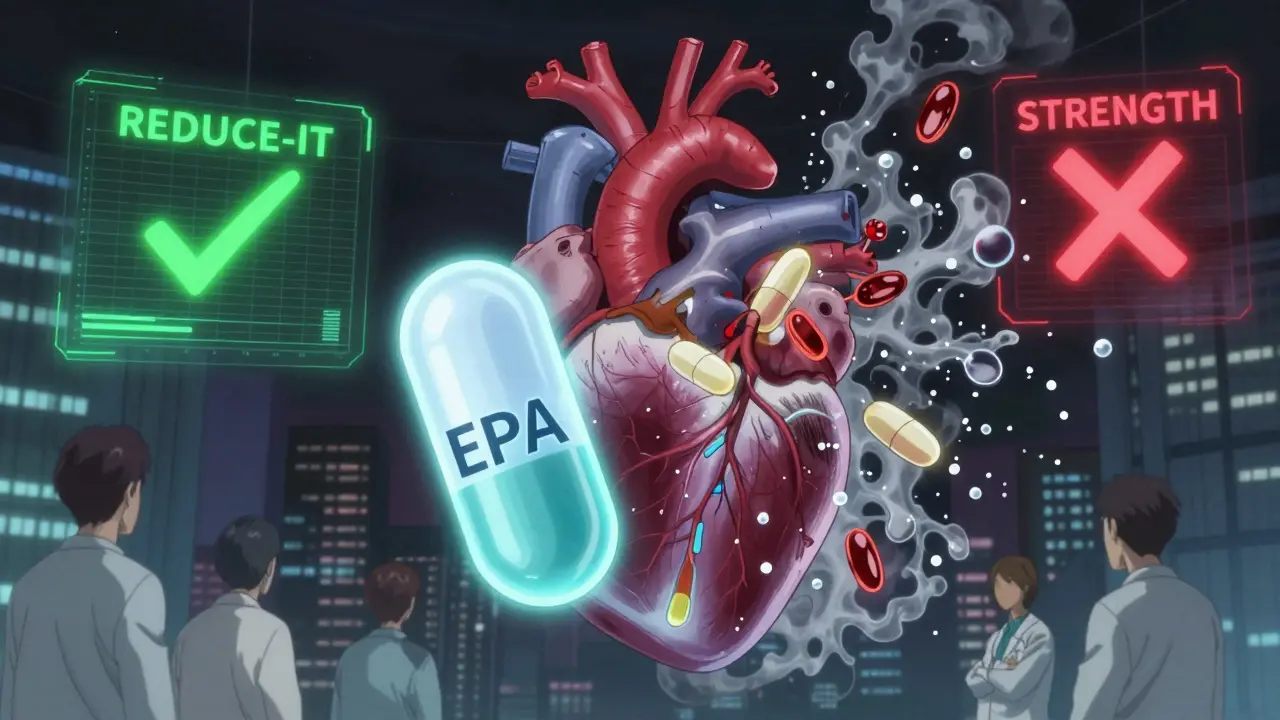
Here’s where things get messy. Two major studies from the last decade give opposite answers.
In 2018, the REDUCE-IT trial shocked the medical world. It followed nearly 8,200 people with high triglycerides and existing heart disease or diabetes. They were given 4 grams a day of a purified EPA-only pill called icosapent ethyl (brand name Vascepa). The result? A 25% drop in heart attacks, strokes, and heart-related deaths. That’s a big deal. This wasn’t a minor tweak - it was a major win.
Then came the STRENGTH trial in 2020. Same dose - 4 grams a day. But this time, they used a mix of EPA and DHA. The outcome? Nothing. No benefit. The trial was stopped early because it was clear the supplement wasn’t helping.
That’s not a typo. One study showed strong results. The other showed nothing. And the only real difference? One had pure EPA. The other had EPA + DHA.
Then there’s the 2023 Cochrane review - the gold standard for pulling together all the best evidence. It looked at 79 trials with over 112,000 people. The conclusion? Long-chain omega-3 supplements (EPA and DHA) have little to no effect on heart attacks, strokes, or death from heart disease.
So which one do you believe?
Prescription vs. Over-the-Counter: Not the Same Thing
Not all fish oil is created equal. And confusing them could cost you money - or worse, your health.
Prescription omega-3s like Vascepa and Lovaza are highly purified, tightly regulated, and given in specific doses. Vascepa is FDA-approved only for people with triglycerides over 150 mg/dL who are already on statins. It’s not for healthy people trying to prevent heart disease. It’s for high-risk patients. And it’s expensive - around $300 a month, even with insurance.
Over-the-counter fish oil? You can buy it at the grocery store. A typical capsule has 300-500 mg of combined EPA and DHA. To hit the 4 grams used in REDUCE-IT, you’d need to swallow 8-12 capsules a day. That’s not practical. And most of these supplements aren’t even tested for quality. Consumer Reports found 12 out of 35 popular brands had oxidized oil - meaning the fats had gone rancid. Rancid fish oil doesn’t help your heart. It might hurt it.
And here’s another thing: most OTC fish oil doesn’t even contain the amount listed on the label. Independent tests show some brands deliver only half the EPA and DHA they promise.
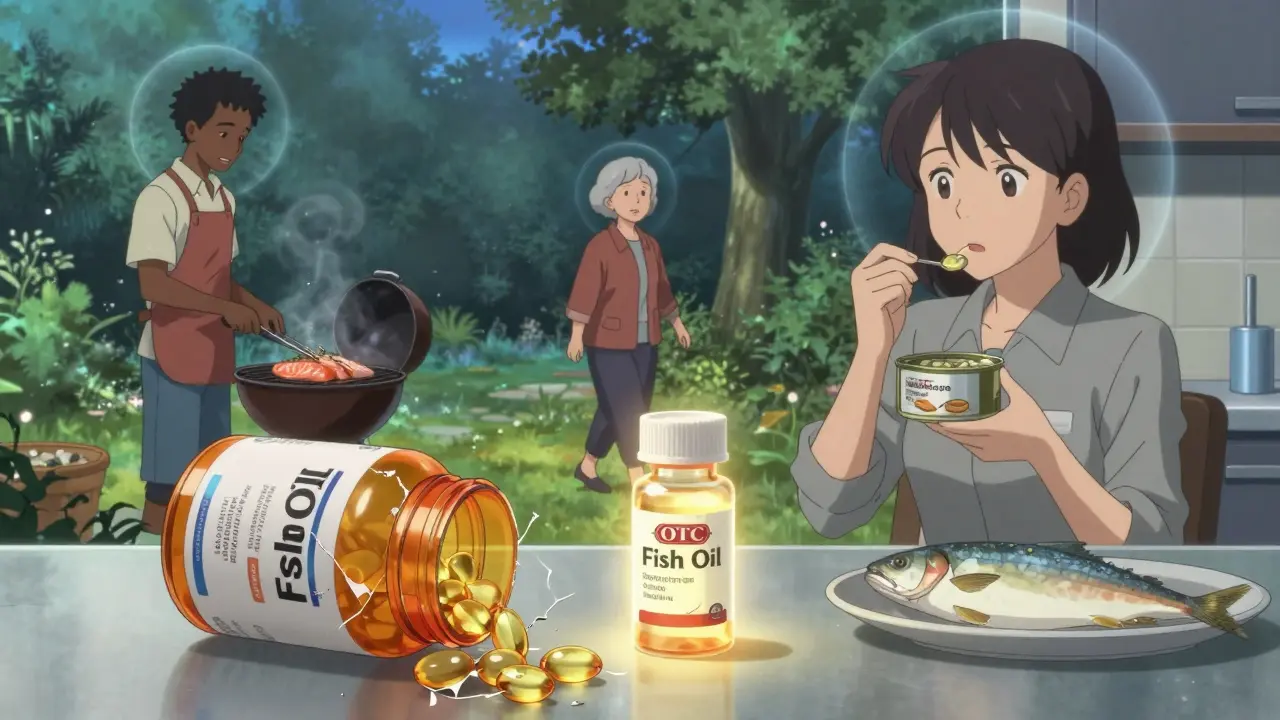
Who Actually Benefits?
If you’re healthy and eating fish twice a week, you probably don’t need a supplement. The American Heart Association says two servings of fatty fish a week gives you about 500 mg of EPA and DHA daily - enough for general heart support.
But if you have:
- High triglycerides (above 150 mg/dL)
- Already had a heart attack or have coronary disease
- Are on a statin and still have high triglycerides
Then you might be a candidate for prescription EPA. That’s the only group where the evidence is strong enough for doctors to recommend it.
There’s also a surprising subgroup: African Americans. In the VITAL trial, people of African descent who took omega-3s had a 77% lower risk of heart attack. Why? Researchers think it might be linked to genetic differences in how the body processes omega-3s. That’s not a reason to start taking fish oil if you’re not in that group - but it shows the benefits aren’t one-size-fits-all.
What About Side Effects?
Fish oil isn’t harmless. At high doses, it can:
- Increase the risk of atrial fibrillation (an irregular heartbeat) - by about 0.4% in large studies
- Thin your blood slightly - not enough to replace blood thinners, but enough to be risky if you’re on warfarin or aspirin
- Give you fishy burps, bloating, or diarrhea - 27% of users report this
And here’s something most people don’t think about: quality. Cheap supplements can contain mercury, PCBs, or other toxins. Reputable brands test for this. Look for third-party certifications like USP, NSF, or ConsumerLab. They don’t guarantee effectiveness - but they do guarantee you’re not getting poison.
What Do Doctors Really Think?
In 2024, a survey of cardiologists on Medscape found that 68% no longer recommend fish oil supplements for people without existing heart disease. That’s a huge shift from just five years ago.
Dr. Deepak Bhatt, who led the REDUCE-IT trial, still stands by EPA for high-risk patients. But Dr. Lee Hooper, who led the Cochrane review, says the evidence doesn’t support widespread use. Even the American Heart Association’s own nutrition chair, Dr. Penny Kris-Etherton, says: “Get your omega-3s from food, not pills.”
The message is clear: Supplements aren’t a magic bullet. They’re a tool - and only for a very specific group of people.
What Should You Do?
Here’s a simple guide based on your situation:
- If you eat fatty fish twice a week: Skip the supplement. You’re already getting enough.
- If you don’t eat fish: Talk to your doctor about whether a low-dose (250-500 mg) EPA/DHA supplement makes sense - but don’t expect miracles.
- If you have high triglycerides or heart disease: Ask your doctor about prescription EPA (Vascepa). Don’t self-prescribe with OTC pills.
- If you’re taking blood thinners or have a history of atrial fibrillation: Talk to your doctor before starting any omega-3 supplement.
The bottom line? Fish oil isn’t dead - but its role has narrowed. It’s not for everyone. It’s not for prevention in healthy people. And it’s not a replacement for statins, blood pressure control, or quitting smoking.
Real heart health comes from eating real food, moving your body, and managing your blood pressure and cholesterol. Omega-3s? They’re a side dish - not the main course.
What’s Next?
The American Heart Association is updating its guidelines in late 2024. Expect clearer rules on who should and shouldn’t take omega-3s. Meanwhile, new trials are underway - like STRENGTH2, testing a new EPA/DHA formula in 2025. Science is still working on this.
For now, stick to the facts: if you’re not in a high-risk group, skip the pills. Eat salmon. Walk daily. Manage your numbers. That’s what actually moves the needle.