Drug Interaction Checker
Enter Your Medications
Your Current List
Enter medications and check for potential interactions.
Every year, thousands of people end up in the hospital because of drug interactions they never saw coming. It’s not always the new medicine that’s the problem-it’s what it’s mixed with. A common painkiller. A vitamin. Grapefruit juice. Even your morning coffee. These hidden clashes can turn a simple treatment into a life-threatening event. The good news? Most of these reactions are completely preventable-if you know how to check.
Why Drug Interactions Are More Common Than You Think
You might think drug interactions are rare, but they’re not. About half of all adverse drug reactions happen because someone didn’t realize their medications were clashing. That’s not a small risk. That’s a daily danger for millions of people taking more than one pill. Take statins, for example. These cholesterol-lowering drugs are among the most prescribed in the world. But if you’re also taking amiodarone (a heart rhythm drug), your risk of a dangerous muscle breakdown called rhabdomyolysis jumps 15 times higher. That’s not a theory-it’s a documented fact. And it’s not just prescription drugs. Over-the-counter pain relievers like ibuprofen can make blood thinners like warfarin dangerously strong, increasing your chance of internal bleeding. Even foods play a role. Grapefruit isn’t just a healthy breakfast choice-it’s a silent saboteur for over 85 medications, including some statins, blood pressure drugs, and anti-anxiety pills. It blocks enzymes in your gut that normally break down these drugs, causing too much to flood into your bloodstream. One grapefruit can cause effects that last over 24 hours.Step 1: Build a Complete Medication List
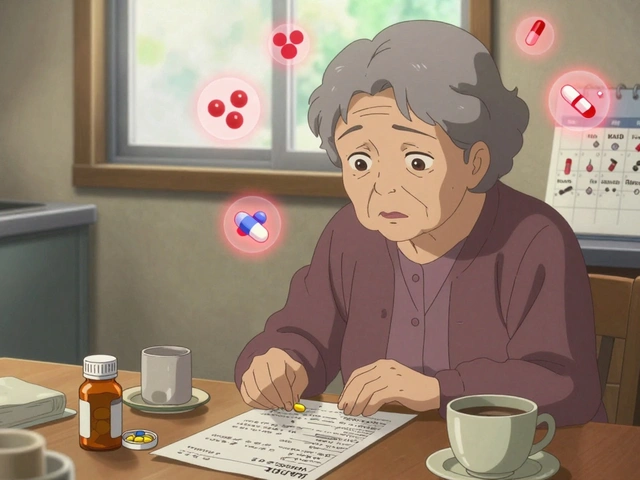
You can’t check for interactions if you don’t know what you’re taking. And most people don’t. A 2022 survey found that nearly 7 out of 10 patients don’t tell all their doctors about every pill, supplement, or herb they use. Start with this: write down every single thing you take, daily or occasionally. That includes:- Prescription drugs (name, dose, how often)
- Over-the-counter meds (like Tylenol, Advil, antacids)
- Vitamins and minerals (even if you think they’re harmless)
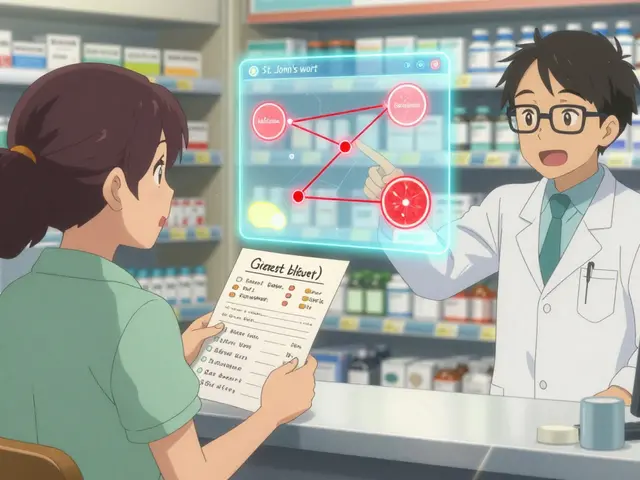
- Herbal supplements (St. John’s wort, turmeric, echinacea)
- Alternative remedies (CBD oil, melatonin, probiotics)
- Recreational substances (alcohol, nicotine, cannabis)
Step 2: Bring Your List to Every Appointment
Doctors don’t know what you’re taking unless you tell them. And they’re busy. They won’t ask unless you lead with it. The BeMedWise Program recommends bringing your physical pill bottles to at least one annual checkup. Why? Because names can be confusing. One person’s "aspirin" might be 81 mg; another’s might be 325 mg. Labels can fade. Pills can be moved between bottles. Seeing the real containers eliminates guesswork. A 2018 study showed that patients who brought their actual meds to appointments had 37% fewer medication errors. That’s not just a nice stat-it means fewer trips to the ER, fewer hospital stays, fewer bad outcomes.Step 3: Ask These Four Questions Before Starting Anything New
When your doctor says, "Here’s a new pill," don’t just say "thanks." Ask:- Can I take this with my other medications? Don’t assume it’s safe just because it’s been prescribed.
- Should I avoid certain foods or drinks? Grapefruit? Alcohol? Caffeine? Dairy? Ask specifically.
- What are the warning signs I should watch for? Muscle pain? Dizziness? Nausea? Unusual bruising? Know what to look for.
- How will this drug work in my body? Understanding the mechanism helps you spot when something’s off.
Step 4: Use a Reliable Drug Interaction Checker
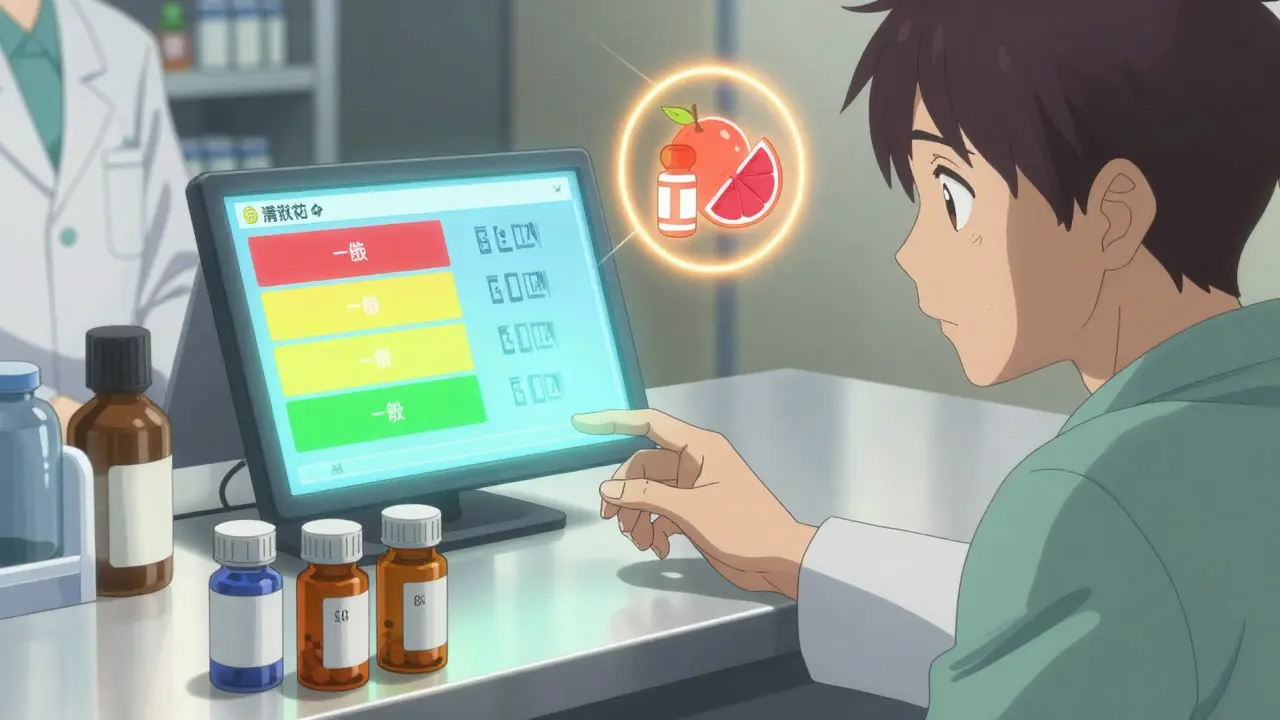
You don’t need to be a pharmacist to check for interactions. Free, trustworthy tools exist. Drugs.com Drug Interactions Checker is one of the most comprehensive. It checks over 24,000 prescription drugs, 7,000 supplements, and 4,000 foods. It’s updated daily and used by over a million people each month. A 2021 study found it caught 92.4% of clinically significant interactions-better than most hospital systems. The University of Liverpool’s HIV Drug Interaction Checker is another standout. Originally built for HIV meds, it now covers hundreds of common drugs and uses a color-coded system: red for dangerous, yellow for caution, green for safe. It even rates the strength of evidence-from strong clinical proof to theoretical risk. Important: These tools are helpers, not replacements for your doctor. They can’t know your kidney function, your age, your genetics, or your full medical history. But they can flag things you might miss.Step 5: Stick to One Pharmacy
Using multiple pharmacies is one of the biggest mistakes people make. Why? Because each pharmacy only sees part of your picture. If you get your blood pressure med from Pharmacy A, your antibiotic from Pharmacy B, and your painkiller from Pharmacy C, none of them can see the full combo. And that’s how dangerous interactions slip through. A 2021 study of 22,000 Medicare patients found that using just one pharmacy reduced serious drug interactions by 31%. Why? Because the pharmacist has your complete history. They can spot a conflict between your statin and your new antibiotic-even if your doctor didn’t. The American Pharmacists Association calls this the "One Pharmacy Rule." It’s simple: get all your prescriptions filled at the same place. Even if it costs a few dollars more. The savings aren’t just in money-they’re in your health.Step 6: Know the Top 7 High-Risk Combinations
Some drug pairs are so dangerous they’re considered medical red flags. Here are the seven most common combinations that land people in the hospital:- Warfarin + NSAIDs (like ibuprofen or naproxen): High risk of bleeding
- SSRIs + MAOIs (antidepressants): Can cause serotonin syndrome-a life-threatening surge in brain chemicals
- Digoxin + Clarithromycin: Can spike digoxin levels, leading to heart rhythm problems
- Statins + Fibrates: Greatly increases risk of muscle damage
- Calcium channel blockers + Protease inhibitors: Can cause dangerously low blood pressure
- Sildenafil (Viagra) + Nitrates: Can cause sudden, fatal drops in blood pressure
- Theophylline + Fluvoxamine: Can cause seizures or heart rhythm issues




Let’s be real - most people don’t even know what’s in their own supplements. I’ve seen folks popping ‘natural’ turmeric with blood thinners like it’s candy. No one checks. No one cares. Until they’re bleeding out in the ER. This guide? It’s not ‘helpful’ - it’s a goddamn lifeline.
You’re not alone if this feels overwhelming. I used to ignore my meds list till my pharmacist called me out - turns out I was doubling up on ibuprofen and my blood pressure med. Took me five minutes to fix it. You got this. Start small. Write one thing down today.
My grandma took grapefruit every morning with her statin. Doctor never mentioned it. She ended up in the hospital with muscle damage. This isn’t theoretical. It’s real. And it’s preventable. Thanks for laying this out so clearly.
so i started writing down everything i take even the melatonin and the cbd oil and like i had no idea how many things i was actually taking like i thought i was just on a few pills but turns out i had like 17 different things and some of them were totally unnecessary like why did i even have that echinacea i bought in 2020
I used to think pharmacists were just there to hand out pills. Then my mom had a bad reaction because her meds weren’t synced across two pharmacies. I switched everything to one place. Best health decision I ever made. Simple. Cheap. Life-saving.
OMG I JUST REALIZED I’VE BEEN TAKING ST. JOHN’S WORT WITH MY ANTIDEPRESSANT 😱 I’M GOING TO THE PHARMACY RIGHT NOW. THANK YOU FOR THIS 🙏
They say ‘use one pharmacy’ like it’s that simple. What about people who use mail-order for chronic meds and local for antibiotics? The system is broken, not the patient. This is corporate control disguised as ‘safety.’
Did you really just say ‘grapefruit juice blocks enzymes’ like it’s some kind of revelation? I’ve been telling people this since 2018. And you think people don’t know about drug interactions? Most of them just don’t care. They’d rather die than admit they need to read a label.
It is, without hyperbole, a matter of profound public health significance that the average individual possesses neither the requisite pharmacological literacy nor the institutional discipline to maintain a comprehensive medication inventory. One must, therefore, conclude that the onus of safety lies not with the pharmaceutical apparatus, but with the conscientious citizen who undertakes the arduous task of self-advocacy.
they put grapefruit in the meds because the government wants you to be sick so they can sell you more pills. the FDA knows about this. they just don't care. and why do you think they want you to use one pharmacy? so they can track you. big pharma is watching.
people who don't take their meds exactly right deserve what they get. if you can't keep track of your pills you shouldn't be on them. this whole guide is just enabling lazy people to stay alive
My cousin in Japan uses a handwritten list and shows it to every doctor. No app. No fancy tools. Just paper and honesty. Sometimes the oldest way is the best.
lol you think the US is the only place this happens? Try Australia. We’ve got people mixing statins with echinacea because some TikTok influencer said it ‘boosts immunity.’ Then they end up in the ICU and wonder why their body’s betraying them.
There’s so much fear in this post - and rightly so. But let’s not forget: most people aren’t trying to be careless. They’re overwhelmed. The system’s broken. We need better tools, not just more reminders. This guide helps - but it shouldn’t be on the patient to fix the system.
I read this while waiting for my prescription. I added three things to my list I’d forgotten. One was a fish oil I took for three years thinking it was ‘harmless.’ Turns out it thins blood. I called my doctor. He said thanks. That’s all it took.