Why Medication Errors Happen When Patients Move Between Care Settings
Imagine you’re discharged from the hospital after a heart attack. You’re handed a stack of new pills - blood thinners, statins, diuretics - and told to take them exactly as directed. But you’re tired, confused, and the nurse didn’t explain what each one does. Back home, you mix up the doses. A week later, you’re back in the ER with dangerous bleeding. This isn’t rare. In fact, medication errors during care transitions are one of the most common causes of preventable harm in healthcare.
According to the Agency for Healthcare Research and Quality (AHRQ), about 60% of all medication errors happen when patients move from one care setting to another - like from hospital to home, or from ICU to a rehab center. These aren’t just small mistakes. They lead to hospital readmissions, emergency visits, and sometimes death. The World Health Organization calls this a global crisis and has made it a top priority under its Medication Without Harm campaign.
The biggest problem? Information gets lost in the shuffle. A patient’s real medication list - the one they’re actually taking at home - often doesn’t match what’s recorded in the hospital system. Maybe the patient forgot to mention their herbal supplement. Maybe the pharmacist didn’t update the community pharmacy’s records. Maybe the nurse didn’t have time to check with the family. These gaps add up fast.
The Four Steps That Actually Work to Prevent Errors
Preventing these errors isn’t about adding more paperwork. It’s about following a clear, proven process called medication reconciliation. This isn’t just a checklist. It’s a safety system with four critical steps that must happen every single time a patient moves between care settings.
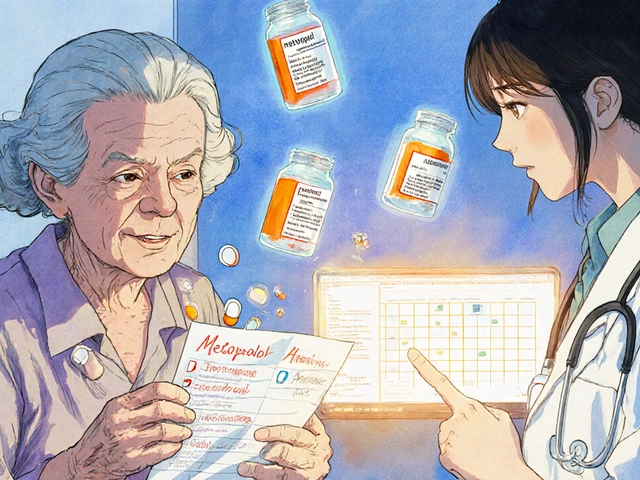
- Create an accurate list of all medications the patient is currently taking - including prescription drugs, over-the-counter pills, vitamins, supplements, and even creams or patches. Don’t just rely on what the patient says. Call their pharmacy. Ask their primary care doctor. Check the state prescription drug monitoring program if available.
- Make a list of the medications the provider plans to prescribe - the ones written in the discharge order or transfer note. This is where EHR systems often fail. Orders might say “continue metformin,” but the patient stopped it three months ago.
- Compare the two lists side by side - look for duplicates, omissions, dosage changes, and dangerous interactions. A common error? Prescribing a new blood thinner while the patient is still on an old one. That’s a recipe for internal bleeding.
- Make clinical decisions and communicate them clearly - decide what to keep, stop, or change. Then make sure the patient, their family, and the next provider all understand the changes. No jargon. No assumptions.
This process isn’t optional. It’s required by The Joint Commission’s National Patient Safety Goals and mandated by Medicare and Medicaid in the U.S. But here’s the catch: only 42% of U.S. hospitals do it well. Most do it poorly because they treat it like a form to fill out, not a safety step.
Technology Helps - But Only If Used Right
Electronic health records (EHRs), barcode scanners, and clinical decision support tools sound like the perfect fix. And they are - when implemented correctly. A 2022 Cochrane review found that hospitals using these tools saw medication errors drop by 48%. But there’s a dark side.
When hospitals first roll out new EHR systems, medication discrepancies actually go up by 18%. Why? Because staff are overwhelmed. They’re learning a new system, rushing through screens, and clicking shortcuts instead of verifying. One study published in JAMA Internal Medicine found that when nurses were trained to take medication histories without clear roles, harmful errors increased by 15%.
The real winner isn’t the software. It’s the Medication at Transitions and Clinical Handoffs (MATCH) toolkit from AHRQ. This isn’t just a tech guide. It’s a full workflow redesign. It tells you who does what, when, and how. Hospitals that used all 159 recommendations in the MATCH toolkit saw a 63% drop in errors. Those relying only on EHRs? Just 41%.
And here’s a surprise: the best technology doesn’t even involve computers. It’s pharmacist-led reconciliation. A 2023 study in the Journal of the American Pharmacists Association showed that when pharmacists lead discharge medication reviews, post-discharge errors drop by 57%, and readmissions fall by 38%. That’s because pharmacists aren’t just checking boxes. They’re talking to patients, asking, “Do you know why you’re taking this?” and catching mistakes others miss.
Why Patients Are Left Out of the Process - And How to Fix It
Most patients don’t know their own medication list. A 2024 Kaiser Family Foundation survey found that 72% of people don’t understand why medication lists matter during hospital transitions. They think it’s just paperwork. But when patients are included, everything changes.
One hospital in Sydney started giving patients a simple printed card before discharge - their updated medication list, with the name, dose, reason, and time to take each pill. They asked patients to read it aloud to a nurse. The result? A 31% drop in post-discharge errors. Patients who could explain their meds were far less likely to take them wrong.
But only 28% of facilities consistently involve patients in reconciliation. Why? Because it takes time. And time is the one thing everyone’s short on. A full reconciliation should take 15 to 20 minutes per patient. In reality, most get 8 to 10.
The fix? Don’t make it a task. Make it a conversation. Ask: “What pills are you taking right now?” Then say, “Let’s check this list together.” Use plain language. Avoid “antihypertensive” - say “blood pressure pill.” Show them the pill bottle. Let them hold it. This builds trust and catches errors before they leave the hospital.
What Happens When You Skip the Process
Skipping medication reconciliation isn’t just risky - it’s expensive. In the U.S., each preventable medication error during transition costs an average of $2,600 in extra care. Multiply that by hundreds of thousands of cases each year, and you get $2.1 billion in avoidable spending.
But the human cost is worse. A 2024 study found that patients who had a medication error during discharge were three times more likely to be readmitted within 30 days. For older adults on 10 or more medications, error rates hit 65%. That’s not a glitch. That’s a system failure.
One real case from a Melbourne hospital: an 82-year-old woman was discharged after pneumonia. Her discharge summary said “continue warfarin.” But she had stopped it two weeks earlier because her doctor switched her to a newer drug. The hospital didn’t check with her GP. She took both. Two days later, she bled into her brain. She survived - but barely.
That’s not an accident. That’s a breakdown in communication. And it’s preventable.
What Works in Real Hospitals - And What Doesn’t
Successful programs don’t rely on tech alone. They rely on people, roles, and routines.
At a large teaching hospital in Adelaide, they assigned a dedicated transition pharmacist to every discharge. The pharmacist met with every patient, reviewed all meds, called the community pharmacy, and gave the patient a printed card with a QR code linking to a video explaining each drug. Within six months, readmissions dropped by 41%.
Another hospital in Brisbane trained nurses to use a simple three-question script: “What meds are you taking at home?” “What did your doctor say to change?” “Can you show me the bottles?” They cut errors by 34% in four months.
On the flip side, hospitals that just added a checkbox to their EHR saw no improvement. Some even saw errors rise. Why? Because staff clicked through the screen without reading. They treated it like a compliance task, not a safety step.
The key difference? Ownership. When pharmacists or nurses are given clear responsibility - and time - to do this work, it works. When it’s just “someone else’s job,” it fails.
What You Can Do Right Now - Even If You’re Not a Doctor
You don’t need to be a nurse or pharmacist to help prevent medication errors. If you’re caring for someone going through a transition, here’s what you can do:
- Make a real list - write down every pill, patch, and supplement your loved one takes. Include doses and times. Keep it in your phone and wallet.
- Ask for the updated list - before discharge, ask the care team: “Can I see the final medication list?” Don’t take their word. Ask for a printed copy.
- Call the pharmacy - don’t assume the hospital sent the script. Call the community pharmacy and confirm what was dispensed.
- Ask the patient to explain it - if they can’t tell you what each pill is for, they’re at risk.
- Follow up - call the patient’s doctor one week after discharge. Ask: “Did the meds change? Are they taking them right?”
These steps take 10 minutes. But they can save a life.
What’s Changing in 2025 and Beyond
The rules are tightening. The 2025 National Patient Safety Goals, released in December 2024, now require hospitals to verify high-risk medications with at least two independent sources - not just one. That means calling the pharmacy AND checking with the patient’s primary care provider.
AI tools are also emerging. MedWise Transition, an FDA-cleared system rolled out in late 2024, uses artificial intelligence to flag mismatches between home meds and discharge orders. In a pilot across 12 hospitals, it cut discrepancies by 41%.
And globally, the WHO’s Phase 2 of Medication Without Harm (launched October 2024) is pushing countries to set measurable targets. By 2027, they want to reduce medication-related harm in high-risk transitions by 30%.
The message is clear: this isn’t going away. It’s becoming mandatory. And the tools are getting better. But the biggest factor remains the same: people paying attention.