What Rosacea Really Looks Like
When your face turns red after a hot cup of coffee, a spicy meal, or even just stress, it might feel like just another blush. But if this happens often, lasts for hours, and doesn’t go away even when you calm down, it could be rosacea. This isn’t just acne or sensitive skin. Rosacea is a chronic skin condition that affects the central part of your face - cheeks, nose, chin, and forehead. It starts with flushing, then often turns into persistent redness, bumps, and visible blood vessels. About 75% of people with rosacea notice flushing first, and if left unmanaged, it can become a permanent red glow that looks like a sunburn that never fades.
Why Your Face Turns Red - It’s Not Just Heat
Normal blushing happens when you’re embarrassed or excited, and it fades in minutes. Rosacea flushing is different. It’s triggered by things like alcohol (especially red wine), hot drinks above 60°C, spicy food with capsaicin, UV rays, or even cold wind. These triggers cause your facial blood vessels to overreact, dilating too much and staying open too long. Dermoscopy shows these vessels as tiny red lines, 0.05 to 0.2mm wide, visible in 85% of cases. The redness isn’t just cosmetic - it’s inflammation. Studies show the red channel intensity on photos of affected skin is 15-25% higher than normal skin. And it’s not just your skin: about half of people with rosacea also get eye symptoms like dryness, burning, or light sensitivity.
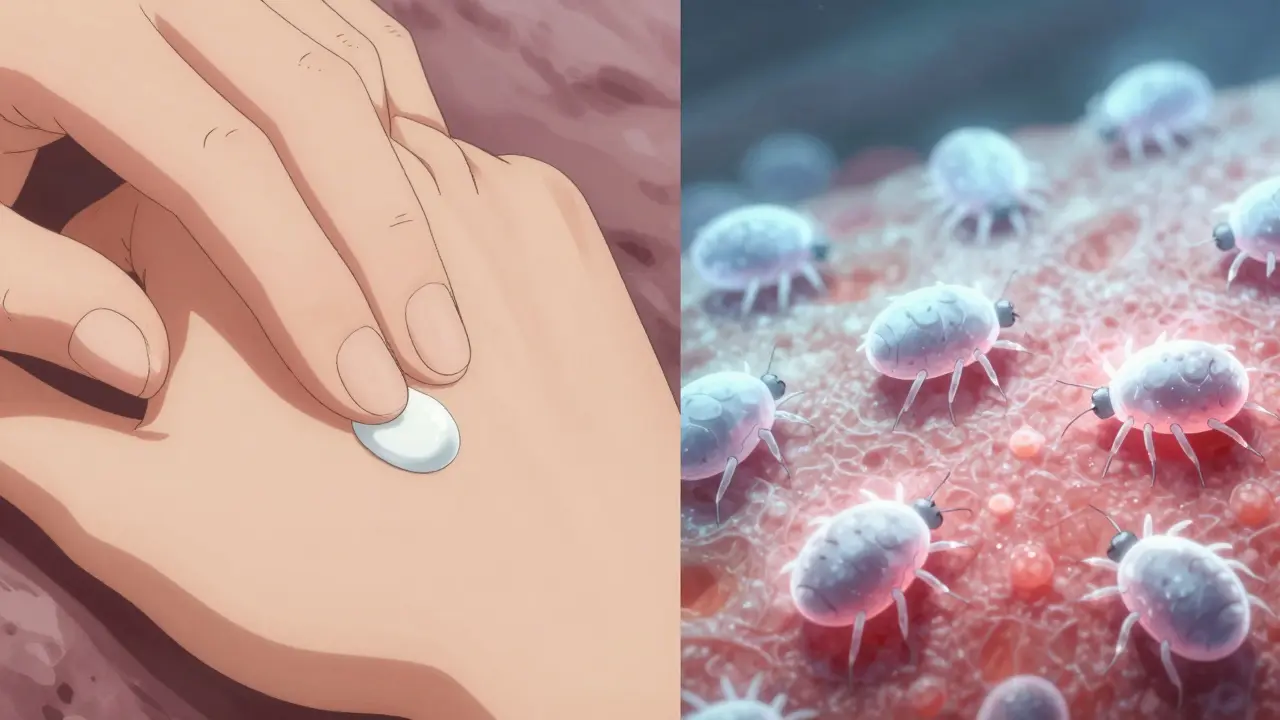
Topical Antibiotics: The First-Line Defense for Bumps and Pimples
While flushing is the early warning sign, many people develop papulopustular rosacea - red bumps and pus-filled spots that look like acne. This affects about half of all rosacea patients. That’s where topical antibiotics come in. They don’t treat the flushing, but they’re the go-to for calming the bumps. Three main options are used: metronidazole, ivermectin, and azelaic acid. Metronidazole gel (0.75%) has been around since the 1980s and reduces bumps by 60-70% after 6-9 weeks. Ivermectin cream (1%), approved in 2014, works better - a 2019 study showed 76% reduction in lesions at 12 weeks, compared to 55% with metronidazole. Azelaic acid (15%) isn’t an antibiotic, but it cuts inflammation and bumps by 68-73% over 15 weeks.
How They Compare: Metronidazole vs. Ivermectin vs. Azelaic Acid
| Treatment | Formulation | Time to Notice Improvement | Reduction in Lesions (12 Weeks) | Common Side Effects | Best For |
|---|---|---|---|---|---|
| Metronidazole | 0.75% gel | 4-8 weeks | 60-70% | Burning (15-25%), dryness | Sensitive skin, first-time users |
| Ivermectin | 1% cream | 4-6 weeks | 76% | Burning (22%), dryness | More severe bumps, Demodex mite involvement |
| Azelaic Acid | 15% gel | 8-12 weeks | 68-73% | Stinging, redness | Those avoiding antibiotics, redness + bumps |
Why It Takes So Long - And Why People Quit
Most people expect results in a few days. But these treatments don’t work like acne spot treatments. You need to use them every day for at least 4 weeks before you see any change. Full results take 12 to 16 weeks. That’s why so many people stop. Studies show only 40-50% stick with it past 3 months. The first few weeks can make things worse - your skin might sting, peel, or get redder. One Reddit user wrote, “First 2 weeks of metronidazole made my face extremely red and flaky - almost quit but glad I stuck with it.” That’s normal. Dermatologists recommend doing a patch test on your jawline for 3 days before applying it all over. If you’re sensitive, start with metronidazole 0.75% instead of stronger versions. Apply it to dry skin, wait 15 minutes after washing, and use only a pea-sized amount for your whole face.

It’s Not Just the Cream - Your Routine Matters Too
Using a topical antibiotic alone won’t fix rosacea. You need to protect your skin barrier. That means ditching harsh cleansers, alcohol-based toners, and fragranced lotions. Use gentle, pH-balanced (5.5-7.0) cleansers and mineral sunscreens with zinc oxide (10-20%). Sun exposure is one of the biggest triggers - even on cloudy days. Many dermatologists now combine topical antibiotics with brimonidine or oxymetazoline gels to reduce redness. Others add ceramide moisturizers to help repair the skin. A 2023 survey found 78% of dermatologists recommend this combo approach. Keep a symptom diary to track your triggers. Did your face flare after wine? After a sauna? After using a new face wash? Writing it down helps you avoid the things that make it worse.
What Doesn’t Work - And What’s Coming Next
Topical antibiotics don’t touch the flushing or the persistent redness. That’s why some people feel like the treatment “didn’t work” - they were hoping for a complete glow-up. They’re great for bumps, not for redness. Newer treatments like Mirvaso and Rhofade target blood vessels directly, but they’re temporary fixes. The future? Combination creams. Galderma’s Phase III trial showed a new ivermectin/hydrocortisone combo reduced lesions by 85% - better than ivermectin alone. But for now, the best approach is simple: use your antibiotic consistently, protect your skin, avoid triggers, and give it time. The global rosacea market is growing fast, but the most effective tool still comes in a small tube you apply twice a day.
Real Talk: What Patients Actually Say
On Drugs.com, ivermectin has a 7.2/10 rating from over 1,200 users. Sixty-two percent say it helped - “After 8 weeks, my bumps dropped 80%.” But 16% say it made things worse. Cost is a real issue - without insurance, you’re looking at $350 a year. That’s why many quit. The National Rosacea Society’s survey of 2,100 people found 45% stopped treatment within 6 months because it took too long, hurt too much, or cost too much. But those who stuck with it? Most saw major improvement. One tip that keeps coming up: “Use less than you think you need.” A pea-sized amount covers your whole face. Too much just irritates. And always, always wear sunscreen.


