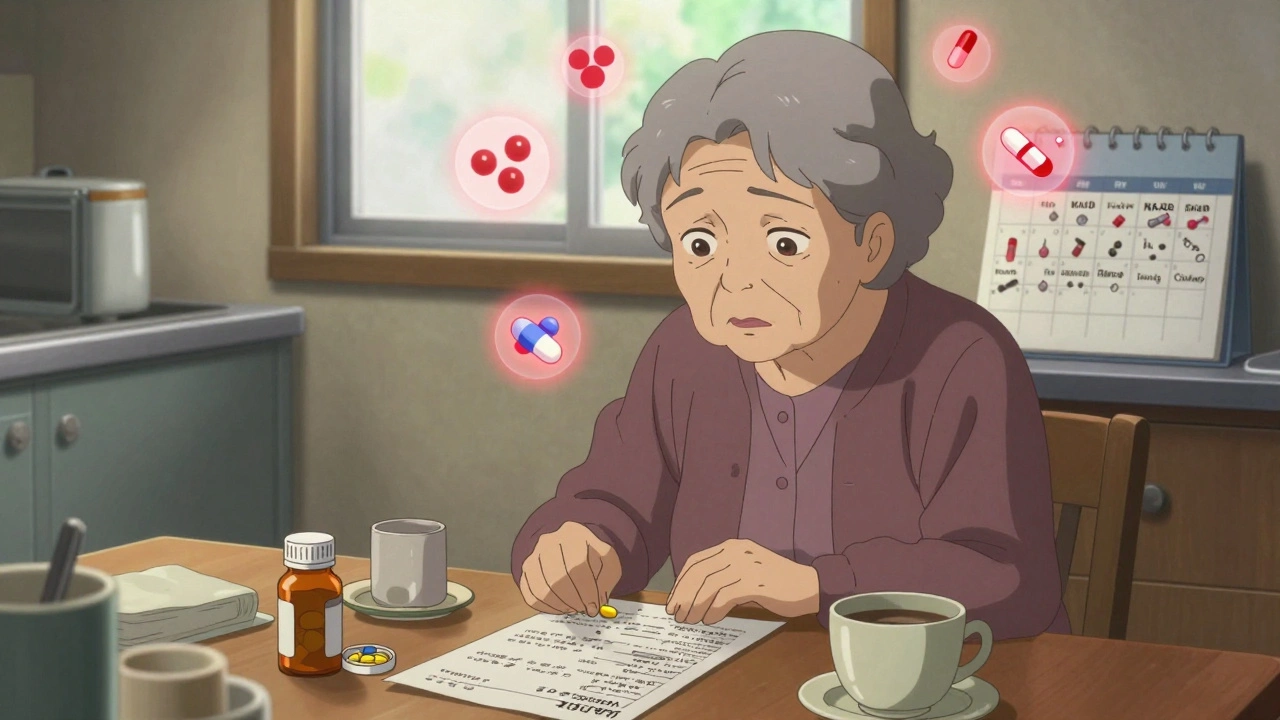
Taking five or more medications at once isn’t just common-it’s becoming the norm for millions of older adults and people with chronic conditions. But what seems like a necessary part of staying healthy can quickly turn into a hidden danger. This is called polypharmacy, and when not managed carefully, it leads to dangerous drug interactions, side effects, falls, hospitalizations, and even death.
What Exactly Is Polypharmacy?
Polypharmacy isn’t just about having a lot of pills. It’s about taking multiple medications at the same time-typically five or more-and not all of them are needed. The World Health Organization (WHO) makes a clear distinction: appropriate polypharmacy means every drug has a real purpose, works for you, and the benefits clearly outweigh the risks. Inappropriate polypharmacy is when you’re taking drugs with no clear reason, drugs that cause more harm than good, or drugs you can’t even remember how to take.According to the American Academy of Family Physicians, 44% of adults over 65 in the U.S. take five or more prescription drugs daily. One in five take ten or more. That’s not just a statistic-it’s your neighbor, your parent, your aunt. And many of those medications weren’t meant to be taken together.
How Do Dangerous Drug Interactions Happen?
Drug interactions don’t happen because someone made a mistake in a lab. They happen because of how care is delivered-and how patients are left to navigate it alone.Imagine this: You see your cardiologist for high blood pressure. They add a new pill. Then you visit your rheumatologist for arthritis and get another. Your primary care doctor prescribes a sleep aid. Your dentist gives you a painkiller. Meanwhile, you’re taking turmeric for inflammation and melatonin for sleep-both bought over the counter. No one has the full list. No one checks how they interact.
This is called care fragmentation. It’s the biggest driver of unsafe polypharmacy. Each provider sees one piece of your health puzzle. Few ask: “What else are you taking?”
Another silent culprit is the prescribing cascade. You take a medication. It causes dizziness. Instead of stopping the original drug, your doctor prescribes another to treat the side effect. Now you’re on two pills for one problem. And the cycle continues.
Then there’s the failure to deprescribe. Many drugs are started during a hospital stay or acute illness-and never reviewed again. A blood thinner prescribed after surgery? A proton pump inhibitor for heartburn? A statin for borderline cholesterol? Years later, you’re still taking them-even if your condition changed, your kidneys slowed down, or you stopped needing them.
What Makes Some Medications More Dangerous Together?
Not all drug combinations are equally risky. Some are ticking time bombs. The Beers Criteria, updated regularly by geriatric experts, lists medications that are especially risky for older adults-and even riskier when mixed.For example:
- Combining benzodiazepines (like diazepam) with opioids increases the chance of respiratory failure.
- NSAIDs (ibuprofen, naproxen) with blood pressure meds can wreck kidney function.
- Anticholinergics (used for overactive bladder, allergies, depression) with antidepressants or antipsychotics can cause confusion, falls, and memory loss.
- Warfarin with aspirin, ibuprofen, or even st. john’s wort can lead to dangerous bleeding.
Even supplements aren’t safe. Garlic, ginkgo, and fish oil can thin your blood. St. John’s wort can make your blood pressure pills, antidepressants, or birth control useless. And most doctors don’t ask about them.
How to Take Control: The 5-Step Safety Plan
You don’t have to accept dangerous medication clutter. There’s a proven way to fix it.1. Build a Master Medication List
Write down every single thing you take-prescription, over-the-counter, vitamins, herbs, supplements. Include:- Drug name and strength (e.g., “Lisinopril 10 mg”)
- Dosage and frequency (e.g., “1 tablet daily”)
- Why you take it (e.g., “for high blood pressure”)
- Who prescribed it (e.g., “Dr. Chen, Cardiology”)
- Special instructions (e.g., “Take with food,” “Avoid grapefruit”)
Update this list every time you see a provider. Bring the actual bottles to your appointment. Don’t rely on memory. Don’t let your doctor guess.
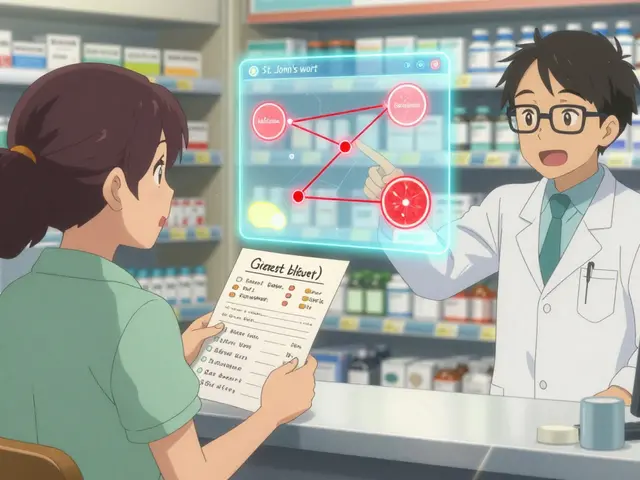
2. Use One Pharmacy
Pharmacists are your hidden safety net. When you use one pharmacy for all your prescriptions, they can run automatic checks for interactions. They’ll flag if your blood pressure pill clashes with your new painkiller. They’ll warn you if that herbal supplement cancels out your thyroid med.Don’t switch pharmacies for convenience. Stick with one. It’s not just about saving time-it’s about saving your life.
3. Ask: “Is This Still Necessary?”
At every visit, ask your doctor: “What are we trying to treat with this? Is it still helping? Could I stop it?”Deprescribing isn’t about taking fewer pills-it’s about taking only the right ones. A 2024 study found that when patients were involved in deciding what to stop, they had fewer side effects and better quality of life.
Some drugs need to be tapered slowly. Stopping a benzodiazepine or antidepressant cold turkey can cause seizures, panic attacks, or rebound insomnia. Never stop on your own. Always work with your provider.
4. Link Medications to Daily Habits
If you forget pills, you’re not lazy-you’re human. The solution isn’t more alarms. It’s tying meds to habits you already do.Take your blood pressure pill right after brushing your teeth. Put your cholesterol med next to your coffee maker. Keep your vitamins in your lunchbox. These simple links make adherence stick without effort.
5. Get Your Team Involved
Managing multiple meds isn’t a solo job. It needs a team: your primary care doctor, pharmacist, nurse, and sometimes a geriatric specialist. Ask if your clinic has a medication review program. Many now offer pharmacist-led reviews where they go through your entire list with you-usually for free.At hospital discharge, insist on a full medication reconciliation. Ask: “What changed? Why? Can I get this in writing?” Many errors happen right after leaving the hospital. A 2023 study showed that patients who received a written updated list had 40% fewer readmissions.
What If You’re Already Overwhelmed?
If you’re taking ten medications and feel like you’re drowning in pills, you’re not alone. The first step isn’t to stop everything-it’s to start asking questions.Ask your pharmacist: “Which of these drugs are most likely to cause problems with each other?”
Ask your doctor: “Is there one drug I could try stopping first? What would we watch for?”
Start with the drugs that have no clear reason, the ones you’ve been taking for years without a check-up, or the ones that cause side effects like dizziness, confusion, or fatigue. Often, removing just one or two can make a huge difference.
When to Call for Help
If you notice any of these, contact your provider immediately:- New dizziness, confusion, or memory lapses
- Unexplained bruising or bleeding
- Severe nausea, vomiting, or diarrhea
- Swelling in ankles or face
- Feeling unusually tired or weak
These aren’t normal aging signs. They’re red flags your body is reacting to a drug interaction.
The Bottom Line
More pills don’t mean better health. In fact, the opposite is often true. Safe polypharmacy means fewer, smarter, better-chosen medications-not just more.You have the right to ask: Why am I taking this? Is it still helping? Can we try stopping it? Your life isn’t a checklist of prescriptions. It’s your life-and you deserve to live it without being weighed down by unnecessary drugs.
Start today: Grab your pill bottles. Write down everything. Bring it to your next appointment. Ask one question. That’s how you take back control.


I’ve seen this play out with my dad-he’s on 12 meds and still takes turmeric like it’s candy. No one ever sat down with him to ask if he actually needed half of them. He just kept taking them because ‘the doctor said so.’ It took a pharmacist noticing he was on three blood thinners to finally start untangling it. I wish more families had this conversation before someone ends up in the ER.
Oh sweet jesus, I’m 32 and I take 4 pills a day and I already feel like a lab rat. At least my pharmacist calls me ‘honey’ and asks if I’ve eaten breakfast. The rest of the medical system treats you like a walking pharmacy inventory. 🙄
Look, I’m a pharmacologist from Mumbai and I’ve reviewed 300+ polypharmacy cases in India alone. Most people don’t realize that 68% of drug interactions happen because of OTC herbs-especially ashwagandha and turmeric, which inhibit CYP3A4 like crazy. And don’t even get me started on people mixing ayurvedic stuff with warfarin. 😤 The WHO guidelines are outdated in emerging markets. You need real-time pharmacokinetic tracking, not some paper list. My clinic uses an AI app that syncs with local pharmacies and flags interactions before the prescription is even filled. If you’re not tech-savvy, you’re literally gambling with your liver.
My mom used to take 8 pills a day. She was always tired, dizzy, forgot her own birthday once. We sat down with her pharmacist and asked, ‘What’s the point of each one?’ Turned out she was still on a statin from 10 years ago-her cholesterol was fine now. Stopped it. She slept better, walked more, started gardening again. It’s not about cutting meds-it’s about cutting the noise. You don’t need to take everything they hand you. Just ask. It’s okay to say no.
One cannot help but observe the profound epistemological failure inherent in the contemporary medical-industrial complex’s reliance on pharmacological band-aids. The very notion of ‘deprescribing’ implies a prior ontological acceptance of pharmaceutical intervention as the default mode of healing-an assumption that is, in fact, culturally pathological. One might argue that the real ‘polypharmacy’ is the epistemic dependency on biomedical authority, wherein the patient’s phenomenological experience is reduced to a pharmacokinetic spreadsheet. The solution, then, is not to manage the pills-but to dismantle the paradigm.
It is both morally irresponsible and clinically negligent to suggest that patients should be entrusted with the authority to question their prescribed regimens. Physicians undergo over a decade of specialized training to determine the appropriate pharmacological interventions. To imply that a layperson, armed with a list of pills and a Google search, can make informed decisions regarding polypharmacy is not only arrogant-it is dangerous. The medical profession exists precisely to prevent such amateur interventions.
Let’s be real: if your doctor doesn’t know what you’re taking, they’re not your doctor-they’re a prescription vending machine. I’ve seen people on 15 meds who can’t even remember their own name. And the worst part? The system rewards prescribing, not stopping. No one gets paid for saying ‘You don’t need this anymore.’ So we keep piling on. It’s not medical care-it’s corporate negligence dressed in a white coat.
Why are we even talking about this? Just take the pills. If you’re too lazy to remember, get a pill organizer. If you’re scared of side effects, don’t be-your doctor knows better than you. This whole ‘ask questions’ thing is just people overcomplicating something simple. I’ve been on 7 meds for 8 years. Still alive. Still walking. Chill out.
Every single one of these ‘solutions’ assumes you have access to a pharmacist who gives a damn, a doctor who has time, and a healthcare system that doesn’t treat you like a billing code. In the real world, most people are lucky if they get a 7-minute appointment and a scrip they can’t afford. This article reads like a luxury pamphlet for the insured. Meanwhile, my uncle in rural Bihar is taking his BP meds with chai because he can’t afford to stop. Stop preaching to the choir and fix the system first.
Ugh I’m so tired of people acting like this is a personal responsibility issue. My grandma’s doctor didn’t even know she was taking ginger capsules because she didn’t think they counted as ‘medicine.’ It’s not her fault. It’s the system. The system that doesn’t ask. The system that doesn’t track. The system that says ‘take this’ but never says ‘when to stop.’ We need a central med record. Like, a real one. Not some PDF your cousin printed out.