Side Effect Reduction Calculator
Your Current Treatment
Combination Therapy Benefits
Potential Benefit: +25-35% less side effects
Based on medical evidence for high blood pressure treatment
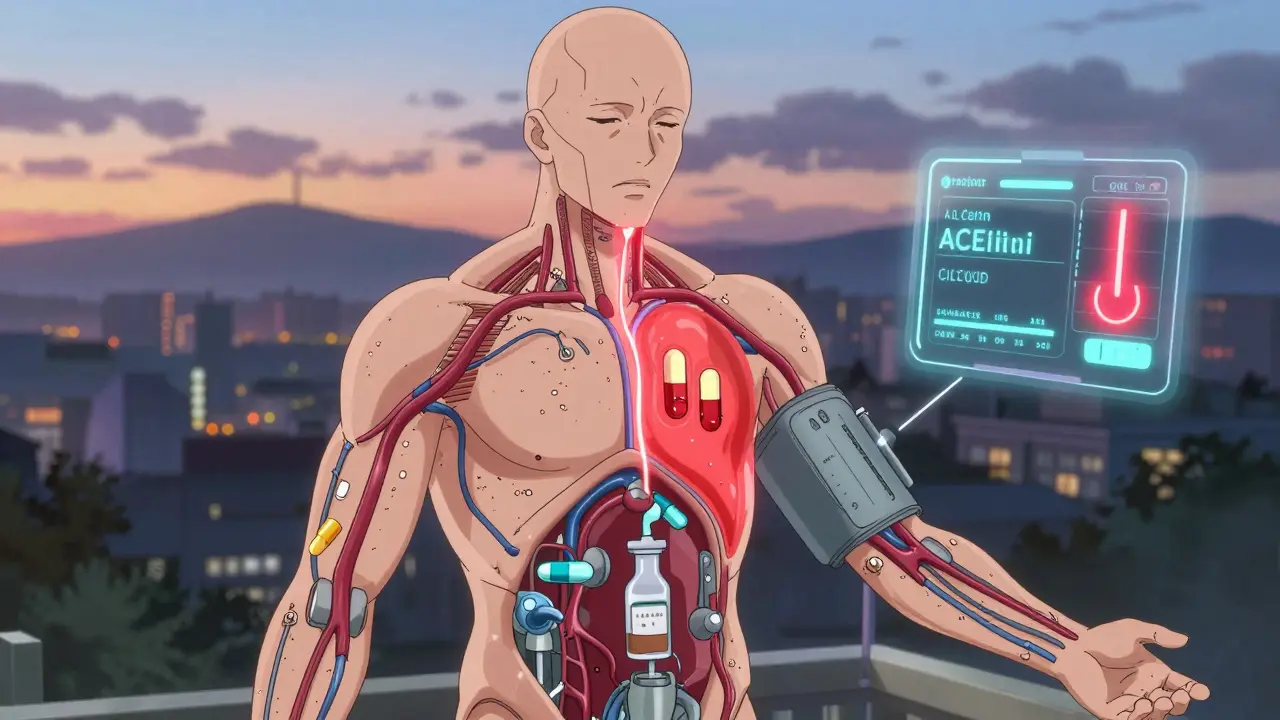
For years, doctors reached for one drug at a high dose to control high blood pressure, diabetes, or even cancer. But that approach often came with a heavy price: dizziness, nausea, swelling, or worse. Now, a smarter strategy is taking over - using combination therapy, where two or more medications are given at lower doses together. It’s not about adding more pills. It’s about working smarter.
Why Lower Doses Work Better Than One High Dose
Think of your body like a machine. When you push one part too hard, it breaks down. That’s what happens with high-dose monotherapy. A 2002 study by Dr. Norman M. Kaplan found that using the full dose of a single blood pressure drug caused 37% more side effects than using half-doses of two different drugs together. The reason? Side effects are often tied to how much of one drug is in your system. Lower the dose, and you lower the risk. In hypertension, combining half-doses of an ACE inhibitor and a calcium channel blocker drops systolic blood pressure by 8.7 mmHg more than the highest single-drug dose. At the same time, swelling (edema) drops from 14.3% to 4.1%, and that annoying dry cough from 9.8% to just 2.3%. It’s not magic. It’s pharmacology. Different drugs hit different targets. Together, they cover more ground without overloading any one system. This isn’t just for blood pressure. In type 2 diabetes, combining metformin 1000 mg/day with an SGLT2 inhibitor like empagliflozin 10 mg/day gives the same HbA1c drop as doubling metformin - but cuts gastrointestinal side effects from 26.4% to 11.7%. That’s a huge win for patients who quit meds because they couldn’t stomach the pills.Real-World Results: Faster Control, Fewer Complications
A 2023 JAMA study tracked over 15,000 patients with high blood pressure. Those who started on a two-drug combo reached their target BP in 63 days. Those on single drugs took 117 days. That’s nearly two months faster. And those extra months? They cost lives. The combo group had 34% fewer heart attacks, strokes, and hospitalizations. In cancer, the numbers are just as striking. A combination of anthracycline and cyclophosphamide at reduced doses works just as well as a high-dose anthracycline alone - but cuts severe neutropenia (dangerously low white blood cells) from 38.7% to 19.2%. Heart damage? Drops from 7.3% to 2.1% over five years. That’s not just about survival. It’s about quality of life. Even more compelling? The UMPIRE trial, published in The Lancet, gave 12,200 people without heart disease a single pill with four drugs at half-doses: aspirin, simvastatin, lisinopril, and atenolol. Five years later, they had 53% fewer heart attacks, 51% fewer strokes, and 49% lower death rates from heart disease. All from pills that were half the usual strength. No one needed to take full doses of anything.
The Pill Burden Problem: When More Pills Backfire
Here’s the catch: taking multiple pills is hard. People forget. They get overwhelmed. A 2024 Diabetes Care survey found 31% of patients on combination therapy stopped within a year - not because it didn’t work, but because they felt buried under pills. Reddit threads from r/Diabetes in early 2024 showed 62% of 1,450 commenters saying they were frustrated with “too many medications.” One wrote: “I take 8 pills a day. I can’t tell if I’m alive because of them or dying from them.” That’s why fixed-dose combinations (FDCs) are changing the game. A single pill with two, three, or even four drugs in one tablet cuts pill burden dramatically. The American Heart Association found 68% adherence for single-pill combos versus 52% for separate pills. Patients say things like, “I only have to remember one thing in the morning.” But FDCs aren’t perfect. They limit flexibility. If you need to adjust one drug’s dose, you can’t - because it’s locked in. That’s why some doctors still prescribe loose combinations, especially early on. But for stable patients? FDCs win.Who Benefits Most - and Who Should Be Careful
Combination therapy shines in moderate to high-risk patients. The European Society of Cardiology recommends it as first-line for stage 2 hypertension. The American Diabetes Association says to start combination therapy within 3-6 months if HbA1c is above 7.5%. Why? Because monotherapy fails in 59% of patients within three years. But not everyone. A 2022 NEJM study found triple-combination therapy raised the risk of acute kidney injury by 1.8 times in older adults with low kidney function (eGFR under 45). For them, less is more. Sometimes, one well-chosen drug at a moderate dose is safer than two. Drug interactions are another hidden danger. The FDA’s adverse event reports from 2023 showed 2,317 complications tied to combination therapy - 48% of them involved older adults on five or more medications. A common mix? Blood thinners, statins, and blood pressure drugs. That’s why pharmacist-led medication reviews are now recommended. One 2023 study showed these reviews cut adverse events by 28%.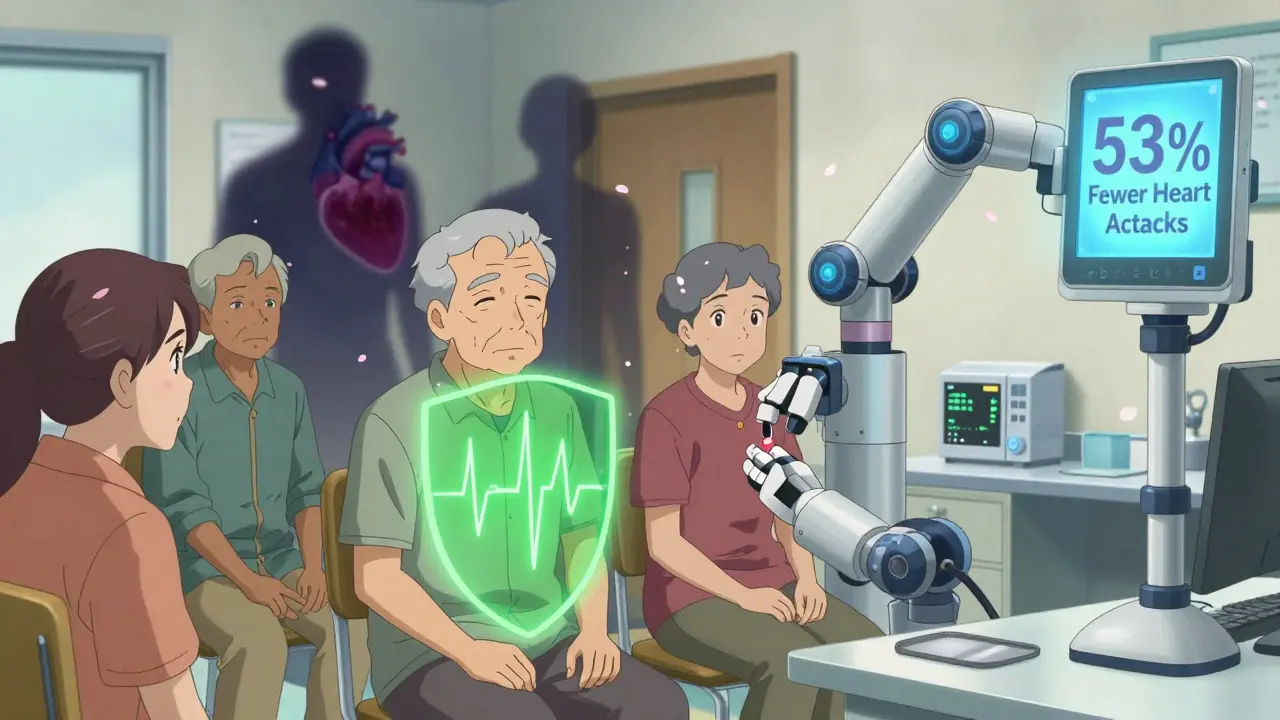
Costs, Access, and the Future
Yes, combination therapy can cost more upfront. A 2024 IQVIA report says the average annual cost is $4,217 versus $2,864 for a single drug. But here’s the flip side: in diabetes, those extra costs are offset by $7,842 less spent on complications like kidney failure, amputations, and hospitalizations. Insurance coverage varies. In the U.S., 37% of uninsured patients walk away from combo prescriptions at the pharmacy. That’s why generic FDCs are exploding. The FDA approved 47 new combination drugs in 2023 - up from 32 in 2022. India’s “polypill” program, which combines four heart drugs in one pill, jumped from 5.3% to 18.7% of prescriptions between 2020 and 2023. The future? We’re moving toward “response-adaptive” therapy. Instead of starting with two drugs, you start with one, monitor how the body responds, then add the next only if needed. A 2024 Harvard study suggests this could cut unnecessary drug exposure by 40% without losing effectiveness. The POLYDELPHI trial, currently enrolling 15,000 people, is testing a five-drug combo at ultra-low doses - each at just 20-30% of normal. If it works, we could prevent heart disease with a pill that barely registers on the scale.What You Need to Know
If you’re on multiple meds or starting treatment for a chronic condition:- Ask if a lower-dose combo could work for you - especially if you’re struggling with side effects.
- Request a fixed-dose combination if you’re taking two or more pills daily.
- Get a medication review from a pharmacist if you take five or more drugs.
- Don’t assume more pills = better results. Sometimes, less is more.
- Track your symptoms. If you feel worse after a combo change, tell your doctor. It might not be the drugs - it might be the mix.
Combination therapy isn’t about throwing everything at the wall. It’s about precision. It’s about balance. And for millions of people, it’s the difference between managing a disease - and living with it.
Is combination therapy safe for older adults?
It can be, but it requires careful monitoring. Older adults, especially those over 75 with reduced kidney function (eGFR under 45), are at higher risk for acute kidney injury with triple-combination therapy. Single-pill combinations with two drugs at low doses are generally safer than multiple separate pills. Always ask for a pharmacist-led medication review if you’re on five or more drugs.
Do combination pills have more side effects than single drugs?
No - they usually have fewer. Side effects often come from high doses of one drug. By lowering each drug’s dose and combining complementary mechanisms, you reduce the chance of dose-related side effects. For example, combining half-doses of an ACE inhibitor and a calcium channel blocker cuts swelling and cough by more than half compared to full-dose ACE inhibitor alone.
Are fixed-dose combinations (FDCs) better than taking separate pills?
For adherence, yes. A 2023 American Heart Association survey found 68% of patients took their single-pill combo regularly, compared to only 52% who took multiple pills. Easier to remember, fewer pills to manage, and fewer chances to miss a dose. But FDCs limit dose flexibility. If your doctor needs to adjust one drug, a loose combination might be better - at least at first.
Why do some doctors still use single-drug therapy first?
Tradition, cost, and caution. Some providers worry about masking side effects or over-treating. Others follow older guidelines. But current standards from the American Diabetes Association, European Society of Cardiology, and others now recommend combination therapy as first-line for moderate-to-high-risk patients. If your doctor hasn’t mentioned it, ask why.
Can combination therapy help me avoid hospital visits?
Yes - and that’s one of its biggest strengths. A 2023 study found patients on initial combination therapy for high blood pressure had 34% fewer cardiovascular events and 22% lower healthcare use. In diabetes, fewer complications mean fewer ER trips for ketoacidosis or foot ulcers. The goal isn’t just to lower numbers - it’s to keep you out of the hospital.
How do I know if combination therapy is right for me?
Ask yourself: Are you struggling with side effects from one drug? Is your condition not improving? Are you taking three or more pills daily? If yes, combination therapy may help. Talk to your doctor or pharmacist. Bring your current meds list. Ask: ‘Would a lower-dose combo be safer or more effective for me?’