Imagine having to take five different pills every day just to manage your high blood pressure, diabetes, and cholesterol. Now imagine taking just one pill that does it all. That’s the power of combination products - and their generic versions are making this easier than ever for millions of patients.
Combination products aren’t just two drugs in one pill. They’re smart, integrated systems - like an insulin pen that combines the drug with a precise dosing mechanism, or a patch that slowly releases medicine through your skin. These aren’t science fiction. They’re real tools used every day by people with chronic conditions. And now, generic versions of these products are hitting the market, offering the same effectiveness at a fraction of the cost.
How Combination Products Make Life Simpler
When you have a chronic illness, sticking to your treatment plan is hard. Life gets busy. Pills get lost. Doses get skipped. Studies show that adherence drops by 26% when you go from taking one pill a day to two. That’s not just a number - it’s people ending up in the hospital because they forgot, got confused, or couldn’t afford it.
Combination products cut through that chaos. Instead of juggling multiple medications, you take one. Take insulin pens, for example. Before they existed, patients had to draw up insulin from a vial with a syringe - a messy, error-prone process. Now, a prefilled pen lets you click, press, and go. Dose accuracy? Within ±5%. Failure rate? Less than 0.1%. That’s not luck - it’s engineering designed for real human lives.
Same with drug-eluting stents. These tiny metal scaffolds, placed in blocked arteries, slowly release medication right where it’s needed. They reduce the chance of the artery clogging again by 30-40% compared to older bare-metal stents. Or nicotine patches - they deliver steady doses of nicotine all day, helping people quit smoking without the spikes and crashes of chewing gum or lozenges.
The result? Patients using combination products are 15-25% more likely to stick with their treatment than those on multiple separate medications. That’s not a small win. It’s life-changing.
Why Generic Versions Are a Game Changer
Here’s the catch: brand-name combination products can cost hundreds - sometimes over a thousand - dollars a month. For many, that’s simply out of reach. That’s where generic versions come in.
Generic combination products aren’t cheap knockoffs. They’re FDA-approved copies that match the brand-name product in every way that matters: same active ingredients, same dosage, same delivery system. The device part - whether it’s a pen, patch, or inhaler - must perform identically. That means the force needed to activate an auto-injector? Still 5-15 Newtons. Dose accuracy? Still within 5%. Failure rates? Still below 0.1%.
The only difference? Price. Generic versions cost 30-80% less. That’s not just savings - it’s access. The FDA found that 23.4% of patients skip doses because of cost. With generics, that number drops. Studies show patients started on generic medications are 8.7 percentage points more likely to stick with their regimen than those on brand-name drugs.
And it’s not just about pills. Generic versions of insulin pens, inhalers, and transdermal patches are now available. For someone with COPD or asthma, a generic inhaler that works just like the brand-name one can mean the difference between breathing normally and ending up in the ER.
The Hidden Challenge: Switching Between Generics
But here’s where things get tricky. Not all generic versions are identical in appearance or feel.
One patient might get a generic insulin pen from Company A one month, then switch to Company B the next. The drug inside? Same. The dose? Same. But the button texture, the click sound, the way it locks - those details can change. For someone with poor eyesight or shaky hands, that’s enough to cause confusion. One Reddit user with diabetes said switching between generic pens reduced his dosing errors from 3-4 per week to almost zero. But another patient on PatientsLikeMe described how switching between generic inhalers made her miss doses because each required a slightly different breathing technique.
This isn’t a flaw in the drugs. It’s a flaw in how pharmacies substitute them. Unlike regular pills, where generic substitution is routine and safe, combination products involve devices. And devices have physical differences. A patient might think they’re getting the same thing - but if the inhaler requires a different inhalation speed or the pen needs a different grip, compliance can drop.
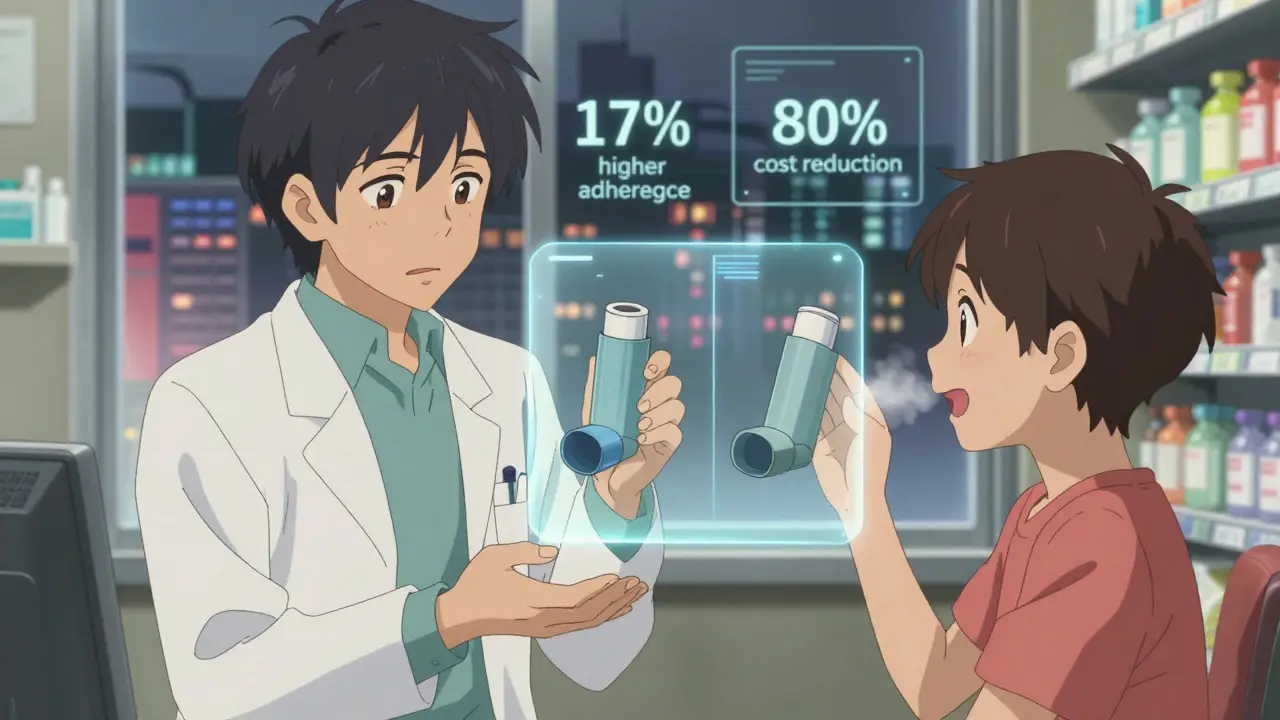
That’s why counseling matters more than ever. A 10-minute conversation with a pharmacist - showing the patient how to use the new device - can boost adherence by 17-22%. It’s not just about telling them it’s the same drug. It’s about showing them how to use the new tool.

What’s Driving the Growth
The global market for combination products hit $127.5 billion in 2022 and is expected to nearly double by 2030. Diabetes treatments alone make up 28% of that market - mostly insulin pens and pumps. But it’s not just chronic diseases. Heart disease, asthma, COPD, and even mental health conditions are seeing new combination products hit the market.
Regulatory changes are speeding things up. The FDA’s Generic Drug User Fee Amendments (GDUFA) have streamlined approval for generics, though combination products still take 18-24 months longer to approve than regular pills. The Inflation Reduction Act of 2022 is pushing Medicare to negotiate drug prices - and that’s creating even more pressure for cheaper alternatives. Experts predict a 40% spike in generic combination product approvals between 2024 and 2026.
Doctors are noticing the difference. Sixty-two percent say they prefer combination products for chronic conditions - not because they’re flashy, but because patients actually take them.
What You Need to Know as a Patient
If you’re on a combination product - brand or generic - here’s what to do:
- Ask if a generic version is available. It’s almost always cheaper. Don’t assume your doctor knows - ask your pharmacist too.
- Don’t assume all generics are the same. If your prescription switches brands, ask if the device works the same way. Look at the instructions. Try it out with your pharmacist.
- Request a demo. Whether it’s a pen, patch, or inhaler, ask for a 5-10 minute hands-on walkthrough. Most pharmacists will do it for free.
- Keep your old device until you’re sure the new one works. Don’t toss it until you’ve tested the new one and feel confident.
- Track your doses. Use a simple app or calendar. Missing a dose? That’s a sign you need to talk to your provider - not just push through.
The goal isn’t just to take your medicine. It’s to take it right - consistently, confidently, and without stress. Generic combination products make that possible. But only if you understand how to use them.
The Bigger Picture
This isn’t just about saving money. It’s about fixing a broken system. Too many people stop taking their meds because it’s too hard, too expensive, or too confusing. Combination products simplify that. Generics make them affordable. Together, they’re a quiet revolution in healthcare - one that doesn’t need flashy ads or new technology. Just better access and better education.
Patients aren’t failing their treatment plans. The system is failing them. Generic combination products are one of the most practical, proven ways to fix that - if we use them right.
Are generic combination products as effective as brand-name ones?
Yes. Generic combination products must meet the same strict standards as brand-name versions. The active drug must be bioequivalent (absorbed the same way), and the device - whether it’s a pen, patch, or inhaler - must perform identically in tests for dose accuracy, reliability, and ease of use. The FDA requires this before approval.
Why do some generic versions feel different to use?
While the drug inside is identical, the device components - like the button, grip, or release mechanism - can vary between manufacturers. These differences are allowed as long as they don’t affect safety or performance. But for patients, especially those with arthritis or vision issues, even small changes can cause confusion. Always ask your pharmacist to demonstrate how to use a new generic version.
Can I switch between different generic versions safely?
You can, but only if you’re properly trained each time. Switching between generic versions of inhalers or auto-injectors without a refresher can lead to dosing errors. If your pharmacy switches your generic, ask for a quick demo. Don’t assume the technique is the same.
How much money can I save with a generic combination product?
Savings vary, but most generic combination products cost 30-80% less than their brand-name equivalents. For example, a brand-name insulin pen might cost $100 per month, while the generic could be under $30. That’s hundreds of dollars saved per year - money that can go toward food, transportation, or other health needs.
Do I need to tell my doctor if I switch to a generic?
Yes. Even though generics are safe, your doctor needs to know what you’re using - especially if you’re switching between different devices. They can help spot issues early and adjust your care plan if you report problems with dosing or side effects.
Next Steps for Better Adherence
If you’re on a combination product, don’t wait until you miss a dose to act. Take 10 minutes today to:
- Check your prescription label - is it a brand-name or generic?
- Ask your pharmacist: “Is there a cheaper generic version available?”
- If you’re switching, ask: “Can you show me how this one works?”
- Set a daily phone reminder to take your medication.
- Write down any confusion or difficulty - and bring it to your next appointment.
Medication adherence isn’t about willpower. It’s about design. Generic combination products are designed to make life easier. You just need to know how to use them.



bro i was taking 5 pills a day for my bp and diabetes and switched to the combo generic last year. life changed. no more pill organizer chaos, no more forgetting one. my mom even started using it and she’s 72 with shaky hands. the pen is way easier than vials. just wish they’d make the buttons louder so i can feel the click.
oh sure, let’s trust the FDA and Big Pharma’s ‘generic’ version. you really think they didn’t tweak the delivery system to make it cheaper? they’ve been doing this since the 90s - slow-release pills that don’t release at all. and don’t get me started on how the pens are made in China now. i’ve seen the supply chain reports. it’s not medicine, it’s a placebo with a sticker.
What we’re seeing here isn’t just a pharmaceutical innovation - it’s a redefinition of care. The human body doesn’t care if a drug is branded or generic. It only responds to consistency, precision, and accessibility. When we remove the friction of cost and complexity, we’re not just improving adherence - we’re restoring dignity. A person shouldn’t have to choose between insulin and groceries. This is systemic empathy engineered into a device.
And yes, the device variations matter. But that’s not a flaw in generics - it’s a flaw in our healthcare delivery model. We treat patients like data points, not people with tactile memory, vision issues, or arthritis. The solution isn’t more pills - it’s more human interaction. A pharmacist taking ten minutes to show you how to use a pen? That’s healthcare.
From a pharmacokinetic standpoint, the bioequivalence thresholds for combination products are stringent - Cmax and AUC must fall within 80–125% of the reference product. But the real bottleneck isn’t the API - it’s the device characterization. FDA requires mechanical validation for auto-injectors: actuation force, dose delivery variance, and failure modes. Generic manufacturers often cut corners on the polymer housing or spring tension, leading to inconsistent actuation. That’s why you see variability in user-reported efficacy - it’s not the drug, it’s the delivery mechanism failing under real-world stress.
And don’t get me started on inhaler actuation timing. A 0.2-second delay in inhalation sync can reduce lung deposition by 40%. That’s not a placebo effect. That’s fluid dynamics.
I’m from South Africa and we don’t have access to most of these combo products - even the brand-name ones. But I’ve seen what they do for people in the US. One guy I met in Johannesburg told me his cousin in Atlanta switched to a generic insulin pen and went from ER visits every month to zero. That’s not magic. That’s justice. We need these tools everywhere. Not just for the rich. For everyone.
Let’s be real - this whole ‘generic combo product’ thing is just a corporate marketing ploy wrapped in virtue signaling. The FDA approves these things faster now because they’re pressured by lobbyists. And who benefits? The pharmacy benefit managers who pocket the difference. Patients? They get devices that feel different, instructions that don’t match, and zero accountability when something goes wrong. And now we’re supposed to applaud this as ‘progress’? Wake up. This isn’t innovation - it’s cost-shifting with a smiley face.
My dad’s a veteran with COPD. He used to pay $400 a month for his inhaler. Last year, his pharmacy switched him to the generic - $28. Same exact drug. Same exact puff count. But the plastic casing was thinner, the mouthpiece smaller. He got frustrated, stopped using it for two weeks. Then his VA pharmacist sat with him for 15 minutes - showed him how to grip it differently, how to breathe slower. Now he’s stable. No ER visits. No panic attacks. It’s not the drug that saves you. It’s the person who teaches you how to use it.
People don’t realize how dangerous this is. Switching generics without counseling? That’s how people overdose. Or underdose. Or have seizures from missed insulin. And no one’s tracking it. No one’s auditing. Just let the pharmacies swap them like candy. It’s reckless. And you’re all acting like it’s a miracle. It’s not. It’s negligence dressed up as savings.
I work in a hospital pharmacy. We get 3-5 generic switch requests a day for combination products. We always offer a demo. Always. But most patients say ‘it’s fine, I’ll figure it out.’ They don’t understand that a 2mm difference in the inhaler’s nozzle can change the entire aerosol pattern. I’ve seen patients come back with pneumonia because they didn’t inhale deep enough. It’s not their fault. It’s ours. We don’t make time. We don’t train. We just dispense.
Let me tell you something - this is the quiet revolution we’ve been waiting for. No hype. No ads. Just better design. A single device that delivers precision, consistency, and affordability. And yes, the device variations matter - but that’s why we need better education, not fear. Patients aren’t failing. The system failed them by making it complicated. Now we’re fixing it. One pen, one patch, one breath at a time. Keep pushing for access. Keep asking for demos. Keep showing up for each other.
USA FTW 🇺🇸 this is why we lead the world in medicine! no other country makes this kind of innovation accessible to the masses. generics? yeah we got ‘em. cheap? hell yeah. safe? FDA says so. if you’re still scared of generics, maybe you should move to a country where they don’t even have insulin. 🤷♀️👏
Just got my generic insulin pen last week. Same as before, but cheaper. My pharmacist showed me how to hold it - I was pressing too hard. Took 30 seconds. No big deal. Don’t overthink it. If it works, use it. If it feels weird, ask for help. Done.