Knowing you’re allergic to a drug isn’t enough. If it’s not written down clearly in your medical records, you could be at serious risk - even in a hospital where staff are trying their best to help you.
Every year, thousands of people in Australia and around the world end up in emergency rooms or intensive care units because someone missed or misunderstood their drug allergy. It’s not always a mistake. Often, it’s because the allergy was recorded vaguely - like “allergic to penicillin” - without details about what actually happened. That’s not enough. And it’s not safe.
Why Vague Allergy Notes Can Be Deadly
When you say, “I’m allergic to ibuprofen,” your doctor might assume you had a rash or stomach upset. But what if you had trouble breathing, your throat swelled, or your blood pressure dropped? That’s anaphylaxis - a life-threatening reaction. If that’s not documented, a nurse might give you another NSAID like naproxen, thinking it’s “safe” because it’s not the same drug. It’s not. Cross-reactions happen.
A 2019 study in the Journal of the American Medical Informatics Association found that incomplete or wrong allergy records contribute to about 6.5% of all medication errors. That’s more than 1 in 15 mistakes. And in the U.S., researchers estimate that better documentation could prevent 1.3 million injuries and 7,000 deaths each year. Those numbers aren’t theoretical. They’re based on real hospital data.
In Australia, hospitals follow the same global standards. The Joint Commission and the National Health and Medical Research Council (NHMRC) require that allergies be clearly listed in your chart - not buried in a paragraph of clinical notes. They need to be front and center. That’s because in an emergency, a doctor might have only 30 seconds to check your records. If the allergy isn’t obvious, it won’t be seen.
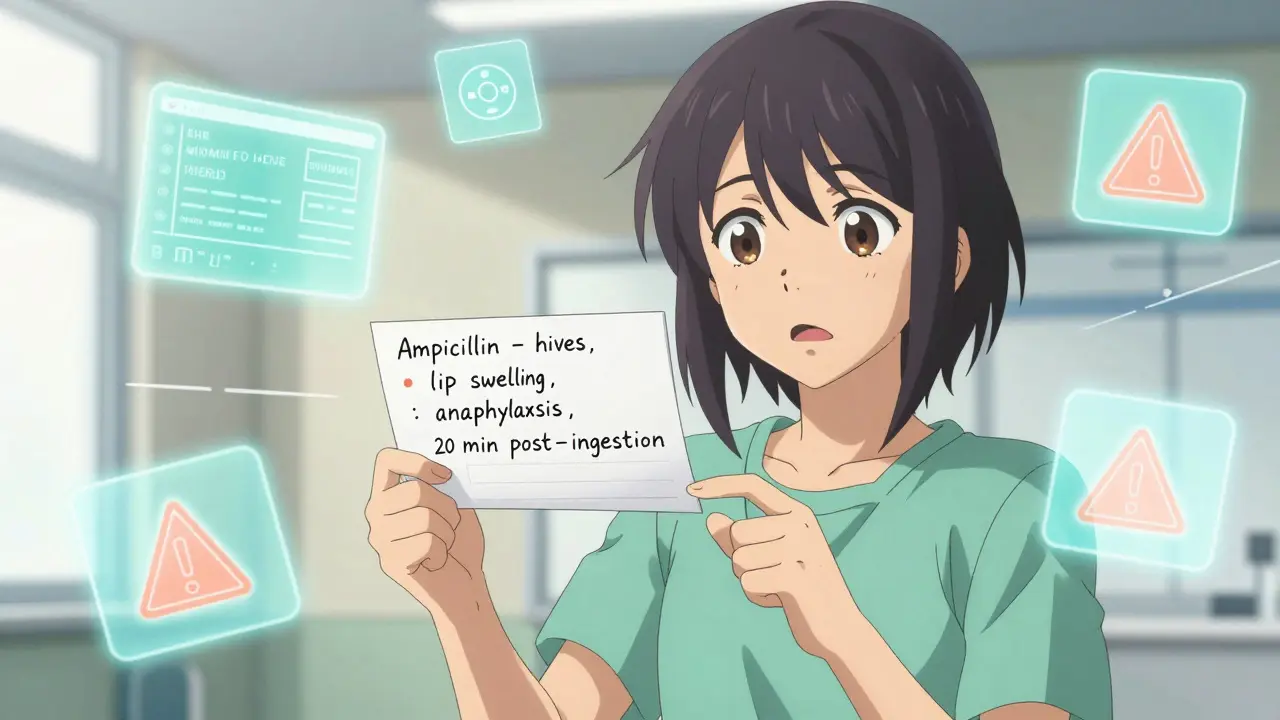
What Exactly Needs to Be Documented
It’s not enough to write “penicillin allergy.” You need four things:
- The exact drug name - use the generic, not the brand. Say “ampicillin,” not “Amoxil.” Say “sulfamethoxazole,” not “Bactrim” or “sulfa.”
- The reaction - what happened? Hives? Swelling? Vomiting? Dizziness? Trouble breathing? Low blood pressure?
- The severity - was it mild, moderate, or life-threatening?
- The timing - when did the reaction happen? Minutes after taking it? Hours? Days later?
Example: “Ampicillin - hives and swelling of lips and tongue, 20 minutes after ingestion, required epinephrine. Diagnosis: anaphylaxis.”
That’s specific. That’s actionable. That’s what saves lives.
Even if you think you’re “just intolerant,” document it. “I get stomach cramps with aspirin” is still important. Some people confuse intolerance with allergy. Intolerance means discomfort, not immune system reaction. But doctors still need to know - they might avoid that drug anyway, or choose a safer alternative.
How Your Doctor Should Record It
Most clinics and hospitals use electronic health records (EHRs) like My Health Record in Australia, Epic, or Cerner. These systems have a dedicated section for allergies. But here’s the problem: many staff still type free text like “allergic to penicillin” instead of selecting the correct coded term from a dropdown menu.
That’s a mistake. Coded entries (like SNOMED CT or LOINC) let computers understand the data. If your record says “penicillin allergy” as code, the system can warn the pharmacist if they try to prescribe amoxicillin - even if it’s called something else.
Best practice? Use both. Select the coded drug from the system’s list, then add a free-text note describing the reaction. That way, the system catches it, and a human reading the record understands the full picture.
Also, if you have no known allergies, it must say so clearly. “NKDA” (No Known Drug Allergies) isn’t optional. It’s required. If it’s missing, doctors assume you might have one - and that can delay treatment.
What You Can Do to Protect Yourself
You’re not just a patient. You’re the most important person in your own safety chain. Here’s how to take control:
- Keep your own list - write down every drug you’ve reacted to, with details. Keep it in your phone or wallet. Update it after every reaction.
- Bring it to every appointment - don’t rely on memory. Even if you’ve been seeing the same doctor for years, allergies change. New reactions happen.
- Ask for confirmation - after your doctor writes something down, ask: “Can you read it back to me?” If they say “penicillin allergy,” correct them if it’s amoxicillin.
- Check your My Health Record - log in at myhealthrecord.gov.au and verify your allergy list. If something’s wrong, contact your GP to fix it.
- Don’t assume past reactions are permanent - about 90% of people who think they’re allergic to penicillin aren’t. Skin tests or graded challenges can confirm this. If you haven’t had a reaction in 10 years, talk to an allergist.
One study at Massachusetts General Hospital found that after a 15-minute structured interview with a nurse using a standard questionnaire, 61% of patients had their allergy records changed - and 185 vague entries were replaced with clear, accurate ones. That’s not just paperwork. That’s life-saving.
Common Mistakes and How to Avoid Them
Here are the top five mistakes patients and providers make - and how to fix them:
- Using brand names - “I’m allergic to Advil.” Fix: Say “ibuprofen.”
- Grouping drugs - “Allergic to all antibiotics.” Fix: List each drug and reaction. Not all antibiotics are the same.
- Forgetting non-drug reactions - “I got sick after the vaccine.” Fix: Vaccines aren’t drugs, but they can cause reactions too. Document them separately.
- Not updating after pregnancy or surgery - New reactions can happen. Always update your record after a hospital stay.
- Thinking “I’ve never had a reaction” means no risk - You can develop an allergy at any time. If you’ve never taken a drug, say “never taken” - don’t leave it blank.
Also, don’t let a nurse or receptionist write your allergy for you. They’re not trained to understand the difference between a rash and anaphylaxis. Tell your doctor or pharmacist directly.
How Technology Is Helping - and Where It’s Falling Short
Electronic systems now alert doctors when they try to prescribe a drug you’re allergic to. In fact, studies show these alerts reduce errors by up to 55%. But here’s the catch: if the allergy is poorly documented, the alert doesn’t work.
Some systems are so sensitive they flag every similar drug - leading to “alert fatigue.” Doctors start ignoring them. That’s why specificity matters. If your record says “ampicillin - anaphylaxis,” the system should warn about amoxicillin and other penicillins - but not about azithromycin or doxycycline.
By December 2023, Australian and global EHRs were required to use the FHIR standard - a modern way of sharing health data. That means your allergy list can now travel with you between hospitals, pharmacies, and specialists. But only if it’s written correctly.
Future tools are coming. AI can now scan clinical notes and pull out allergy details with 85% accuracy. But it can’t guess. It needs clear, consistent data to work.
What Happens If It’s Not Done Right?
Failure to document properly isn’t just a paperwork issue - it’s a legal and safety failure. In Australia, hospitals can be audited by the Australian Commission on Safety and Quality in Health Care. If they find missing or inaccurate allergy records, they can be fined or lose accreditation.
But the real cost isn’t to the hospital. It’s to you. A missed allergy can lead to:
- Emergency intubation
- ICU admission
- Permanent organ damage
- Death
There’s no second chance in anaphylaxis. You can’t say “I didn’t know” after the fact. That’s why documentation isn’t optional. It’s non-negotiable.
Final Checklist: Your Drug Allergy Record
Before your next appointment, check this list:
- Is every drug listed by its generic name?
- Does each entry include the exact reaction?
- Is the severity clearly stated?
- Is there a note for every drug you’ve never taken?
- Is “No Known Drug Allergies” written if true?
- Have you reviewed your My Health Record this year?
If you can answer yes to all of these, you’re doing better than 70% of patients. Keep going. Your life depends on it.
What if I’m not sure if I’m really allergic or just had a side effect?
Many people think they’re allergic when they had a side effect - like nausea or a headache. True allergies involve the immune system and usually include hives, swelling, trouble breathing, or low blood pressure. If you’re unsure, ask your doctor about a referral to an allergist. Skin tests or oral challenges can confirm whether you’re truly allergic. Up to 90% of people who think they’re allergic to penicillin aren’t - and can safely take it again.
Can I remove an allergy from my record if I outgrew it?
Yes. Allergies can fade over time, especially with drugs like penicillin. If you haven’t had a reaction in 10+ years and have no other risk factors, talk to your doctor. They can refer you for testing. If the test is negative, your record can be updated to reflect that you’re no longer allergic - and you’ll have more treatment options in the future.
Do I need to tell every new doctor about my allergies?
Always. Even if you have a My Health Record, not all clinics or hospitals can access it - especially in emergencies. Bring your own list. Say it out loud. Ask them to confirm it’s in their system. Don’t assume it’s already there.
What if my allergy is listed wrong in My Health Record?
Log in to your My Health Record account and check the allergy section. If it’s incorrect, contact your GP or pharmacist and ask them to update it. You can also submit a request directly through the portal. Don’t wait - incorrect records put you at risk every time you see a new provider.
Are food allergies the same as drug allergies in medical records?
No. Food allergies are documented separately from drug allergies. But both are critical. If you have both, make sure each is clearly labeled. Some systems combine them - which can cause confusion. Always specify: “Drug: amoxicillin - anaphylaxis” and “Food: peanuts - anaphylaxis.”




so i read this and i’m like… wait, so if i said ‘allergic to ibuprofen’ but i just got a stomachache, does that mean i’m a walking time bomb? lol. i’ve been saying that for years. maybe i should’ve written ‘got a tummy ache once in 2012 after advil’… but who has time for that?
As a public servant who has seen the consequences of poor documentation in emergency response, I must commend this article for its clarity and urgency. In India, where health infrastructure varies drastically across regions, precise allergy records are not merely a best practice-they are a lifeline. Let us not treat medical safety as optional bureaucracy. This is civil responsibility.
Oh wow, a whole 2000-word essay on how to write ‘allergic to penicillin’ properly. Meanwhile, in the UK, we’ve got nurses who can’t spell ‘anaphylaxis’ and EHRs that crash if you look at them funny. At least your system has a dropdown. We just yell louder when the meds come out.
i’m so tired of people saying ‘i’m allergic to penicillin’ like it’s a personality trait. i had a doc once who wrote ‘allergy: drugs’ in my chart. i swear to god, i almost died because they gave me something ‘similar’ and i had to scream ‘NO, NOT THAT ONE, THE BLUE ONE!’ while the nurse looked at me like i was being dramatic. also, typo: ‘anaphylaxis’ has 2 L’s. just saying.
This entire piece reads like a marketing brochure for Epic EHR. Let’s be real: 90% of patients don’t know what SNOMED CT is, and 80% of providers don’t care. The real problem is systemic neglect, not vague entries. Also, ‘NKDA’ is not a magic spell. It’s a liability shield for hospitals. You think your My Health Record saves lives? Try using it when you’re unconscious in a rural ER with no internet.
THIS IS WHY PEOPLE DIE. STOP BEING LAZY. If you had a reaction, WRITE IT DOWN. If you don’t know what it was, GO TO A DOCTOR. Don’t wait until you’re in the ER gasping for air because someone thought ‘sulfa’ and ‘penicillin’ were the same thing. I’ve seen it. It’s not dramatic. It’s horrifying. Update your damn record today.
Let’s not pretend this is about safety. It’s about liability avoidance disguised as patient empowerment. Hospitals want clean records so they don’t get sued, not because they care if you live. And the ‘90% of people aren’t really allergic to penicillin’ stat? That’s from industry-funded studies. The real risk is overdiagnosis and unnecessary antibiotic use. You’re being manipulated into compliance.
The essence of this matter transcends mere medical documentation; it speaks to the fundamental duty of the individual toward self-preservation in an increasingly mechanized healthcare ecosystem. To neglect the precise articulation of one’s physiological boundaries is not merely negligence-it is an abdication of personal sovereignty in the face of institutional entropy. One must, therefore, treat the allergy record not as a form to be filled, but as a covenant with one’s own biological integrity.
lol at people who say ‘i’m allergic to antibiotics’ like it’s a club membership. honey, you don’t get to say that unless you’ve had anaphylaxis. i had a friend who got hives from cipro and called it ‘antibiotic allergy’-then went on to take amoxicillin 3 years later and ended up in ICU. don’t be that person. be specific. or at least, don’t be the reason someone else dies.
i just opened my my health record and it says ‘allergic to everything’ and i didn’t even put that there. who even did that?? my dentist?? i’ve never had a reaction to anything except maybe coffee. now i’m scared to go to the hospital. also, i’m pretty sure ‘anaphylaxis’ is spelled with an ‘e’ not an ‘a’? idk i’m tired.
Thank you for writing this. I used to think my mild rash from amoxicillin wasn’t a big deal. Now I know it was. I updated my record last week. I also told my mom, my sister, my roommate, my dog (he’s a good listener). I feel like I just gave myself a superpower. We’re all just trying to survive this broken system. Small steps matter.
THIS IS A GOVERNMENT CONTROL TACTIC. They want you to document everything so they can track your body like a drone. Who says you need to tell them your allergies? Maybe your ‘allergy’ is just your body rejecting their poison. The real danger is the pharmaceutical industry pushing drugs and making you scared to question them. Don’t trust the system. Trust your gut.
just updated my record with all my reactions-hives from sulfa, dizziness from codeine, stomach cramps from aspirin. felt weird saying it out loud to my doctor but she smiled and said ‘thank you.’ we’re all just trying to keep each other alive. 🙏❤️
One thing I wish more people knew: if you’re unsure if it was an allergy or just a side effect, get tested. I thought I was allergic to penicillin because I got a rash as a kid. Turned out I wasn’t. Now I can take the meds I need without worrying. Don’t let fear hold you back from better care. Talk to an allergist. Seriously. It’s one appointment. Could change your life.