When you’re past menopause, your body doesn’t just stop changing-it starts reacting differently to the medicines you take. What worked at 45 might not be safe at 65. And if you’re taking four, five, or even six prescriptions a day, the risk of something going wrong goes up fast. This isn’t about fear. It’s about facts. About how your liver processes drugs differently now. About how your bones, heart, and brain have changed. And about how some medications that helped before could now be doing more harm than good.
Why Your Medications Need a Reset After Menopause
Your hormones shift after menopause, and that changes how your body handles every drug you swallow, patch, or inject. Estrogen drops. Liver metabolism slows. Kidney function declines. Fat increases. Muscle mass decreases. These aren’t minor tweaks-they’re major shifts in how your body absorbs, breaks down, and gets rid of medicines. For example, oral estrogen is processed by the liver first. That means it puts extra stress on your liver and raises your risk of blood clots. But if you switch to a patch or gel, the estrogen goes straight into your bloodstream. No liver trip. No extra clotting risk. That’s why transdermal estrogen is now the preferred choice for most post-menopausal women, especially those with a history of clots or high triglycerides. And it’s not just hormones. Blood pressure meds, cholesterol drugs, diabetes pills, pain relievers-they all behave differently in a post-menopausal body. A drug that was fine at 50 might cause dizziness, falls, or stomach bleeding at 70. That’s why a medication list that worked five years ago needs a fresh look today.The Hidden Danger: Taking Too Many Pills
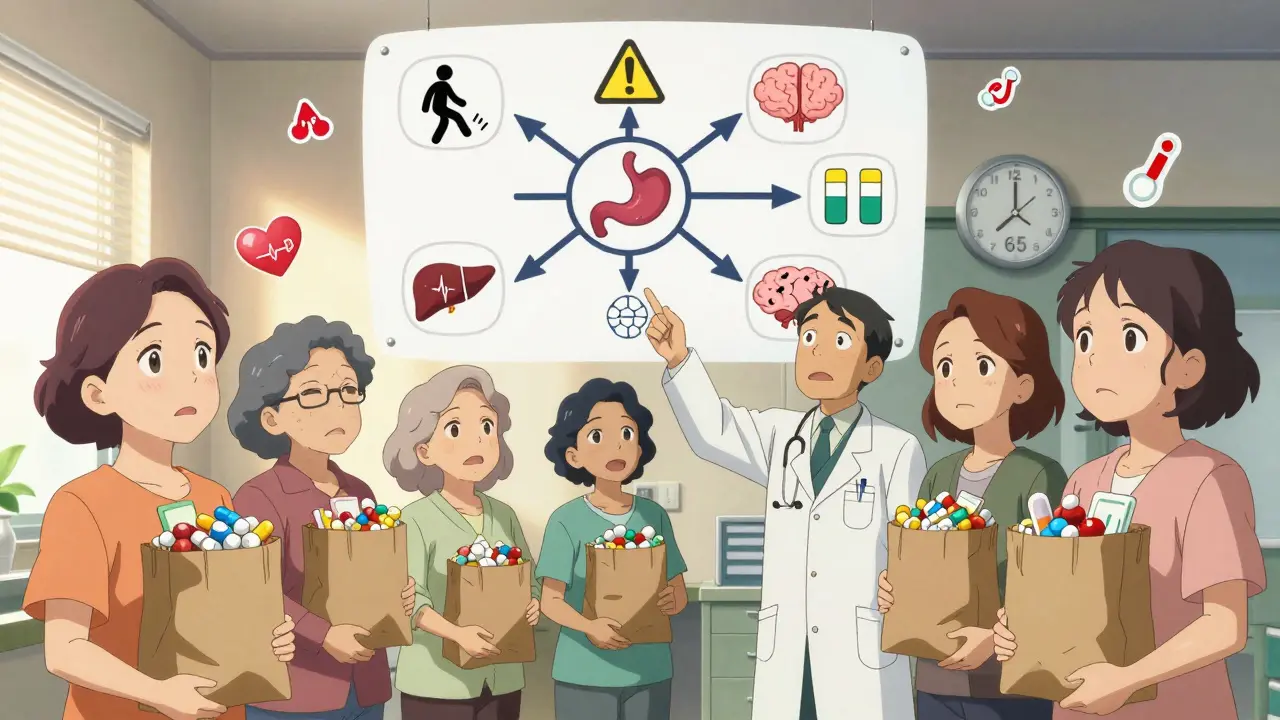
About 44% of women over 65 are taking five or more prescription drugs. That’s called polypharmacy. And it’s not just common-it’s dangerous. Every extra pill adds risk. One study found that women on five or more medications are 2.5 times more likely to be hospitalized for an adverse drug event than those on two or fewer. The problem? Many of these prescriptions come from different doctors. Your cardiologist prescribes a beta-blocker. Your rheumatologist adds an NSAID. Your primary care doctor gives you a sleep aid. No one’s looking at the whole picture. And that’s how you end up with a 72-year-old woman on diclofenac (an NSAID), simvastatin, enalapril, and atenolol-then develop a bleeding ulcer because the NSAID wasn’t stopped, even though her doctor told her to. The solution? A medication review. Not once a year. Not when you’re sick. Every time you see a new doctor, bring every pill, capsule, vitamin, and herbal supplement you take. Put them all in a brown bag. Let the doctor see it. Ask: “Which of these are still necessary?”Hormone Therapy: What’s Safe Now?
Hormone therapy isn’t off the table-but the rules have changed. The old idea that estrogen protects your heart? That’s outdated. The Women’s Health Initiative study showed that combined estrogen-progestin therapy increased breast cancer risk by 24% after five years. It also raised stroke and blood clot risk. That’s why the U.S. Preventive Services Task Force says: don’t use it to prevent heart disease or osteoporosis. But if you’re having hot flashes, night sweats, or vaginal dryness that’s wrecking your sleep and quality of life? Hormone therapy can still help. Just do it right.- Use the lowest dose for the shortest time possible.
- Choose transdermal estrogen over pills if you have any clotting risk.
- Never start hormone therapy after 60 or more than 10 years past menopause. The risks rise sharply after that.
- If you’ve had a hysterectomy, estrogen alone is safer than estrogen-plus-progestin.
- Avoid tibolone. It reduces fractures but increases stroke risk by 58%.
Non-Hormonal Options That Actually Work
You don’t need hormones to manage hot flashes. SSRIs and SNRIs-antidepressants like paroxetine, venlafaxine, and escitalopram-cut hot flash frequency by 50-60%. They’re FDA-approved for this use. But they come with trade-offs: sexual side effects in 30-40% of users, nausea, and weight gain. Gabapentin and pregabalin, originally for nerve pain, also reduce hot flashes. They’re less effective than hormones but safer for women with a history of breast cancer or blood clots. And don’t overlook non-drug options. Clinical trials show that cognitive behavioral therapy (CBT) for hot flashes reduces their impact as much as low-dose hormones. Regular exercise, especially walking and strength training, helps too. Cooling techniques, like wearing layers and keeping your bedroom at 65°F, aren’t fancy-but they work.Medications to Avoid After 65
The Beers Criteria, updated in 2019, lists 30 drugs that should be avoided in older adults. Many are still prescribed routinely. Here are the big ones:- Long-acting benzodiazepines (like diazepam): Increase hip fracture risk by 50%. Avoid completely.
- Nonsteroidal anti-inflammatories (NSAIDs) (like ibuprofen, naproxen): Raise risk of stomach bleeding, kidney damage, and heart failure. Use only if absolutely necessary and for the shortest time.
- Anticholinergics (like diphenhydramine, oxybutynin): Cause confusion, memory loss, constipation, and urinary retention. Found in many sleep aids and bladder meds.
- First-generation antihistamines: Same risks as above. Not safe for older brains.
- Oral estrogen with progestin: Only for symptom relief, never for prevention.

Deprescribing: Taking Pills Off the List
Getting off a medication isn’t as simple as stopping it. Some drugs need to be tapered. Others need replacement. This is called deprescribing-and it’s one of the most important steps you can take. A 2019 WHO report found that structured deprescribing reduces medication burden by 1.4 drugs per person and cuts adverse events by 33%. But it takes planning.- Start with one drug at a time.
- For antidepressants or anti-anxiety meds, taper over 4-8 weeks.
- For benzodiazepines, go slow: 8-12 weeks.
- Track symptoms. If anxiety or insomnia returns, you might need a different approach.
- Use the START/STOPP criteria: a tool doctors use to spot medications that are either unnecessary or missing.
How to Stay Safe Every Day
You don’t need to be a pharmacist to manage your meds safely. Just follow these simple steps:- Keep a current list of every medication, including doses, times, and why you take them. Update it after every doctor visit.
- Use a pill organizer with alarms. Studies show it cuts errors by 81%.
- Never take two pills at once just because you missed one. Check the label or call your pharmacist.
- Ask your pharmacist: “Is this safe with everything else I take?” They’re trained for this.
- Get your blood tested regularly. Some drugs (like statins or diuretics) need monitoring.
- Don’t ignore side effects. Dizziness? Confusion? Nausea? Fatigue? These aren’t just “getting older.” They might be your meds.
What’s Next for Medication Safety
New tools are coming. AI systems are being tested to flag dangerous drug combinations before they’re prescribed. Pharmacogenomic testing (checking your genes to see how you metabolize drugs) is becoming more common-especially for drugs like tamoxifen, where your genes affect whether it works or not. The NIH is funding $25 million in research to find better non-hormonal options for menopause symptoms. And the FDA now requires drug labels to include specific warnings for post-menopausal women. But the biggest change? It’s not a new drug. It’s a new mindset. Medication safety isn’t about taking more pills. It’s about taking the right ones-and only the ones you truly need.Is hormone therapy safe for post-menopausal women?
Hormone therapy can be safe for managing menopause symptoms like hot flashes and vaginal dryness, but only under specific conditions. It should be used at the lowest effective dose for the shortest time possible. Transdermal estrogen (patch or gel) is safer than oral forms, especially for women with a history of blood clots or high triglycerides. It should not be used to prevent heart disease or osteoporosis. Women with a uterus need progesterone to protect the uterine lining, but those without a uterus can use estrogen alone, which carries lower breast cancer risk. Starting hormone therapy after age 60 or more than 10 years after menopause increases risks and is generally not recommended.
Why is polypharmacy dangerous for older women?
Polypharmacy-taking five or more medications-increases the risk of harmful drug interactions, side effects, and hospitalizations. As women age, their liver and kidneys process drugs slower, making them more sensitive to medications. Taking multiple drugs from different doctors often leads to duplication, unnecessary prescriptions, or dangerous combinations. Studies show that women on five or more drugs are 2.5 times more likely to be hospitalized for an adverse drug event. The risk is even higher with over-the-counter drugs, supplements, or herbal products that aren’t disclosed to providers.
What medications should post-menopausal women avoid?
Post-menopausal women should avoid long-acting benzodiazepines (like diazepam), nonsteroidal anti-inflammatories (NSAIDs like ibuprofen or naproxen) for long-term use, anticholinergic drugs (like diphenhydramine or oxybutynin), and first-generation antihistamines. These increase risks of falls, fractures, confusion, memory loss, and stomach bleeding. Oral estrogen combined with progestin should only be used for symptom relief, not prevention. Always check the Beers Criteria, a list of potentially inappropriate medications for older adults, with your doctor.
Can I stop taking my medications on my own?
No. Stopping certain medications suddenly can cause serious withdrawal effects. Antidepressants, blood pressure drugs, and benzodiazepines must be tapered slowly under medical supervision. Even supplements or over-the-counter drugs can cause rebound symptoms or dangerous interactions if stopped abruptly. Always talk to your doctor before stopping any medication. They can help you create a safe plan to reduce or replace drugs that are no longer necessary.
What are safe alternatives to hormone therapy for hot flashes?
Several non-hormonal options are effective. SSRIs like paroxetine and SNRIs like venlafaxine reduce hot flash frequency by 50-60% and are FDA-approved for this use. Gabapentin and pregabalin also help, especially for women who can’t use hormones. Cognitive behavioral therapy (CBT) has been shown to reduce the impact of hot flashes as much as low-dose hormones. Lifestyle changes-like wearing breathable clothing, keeping your environment cool, avoiding triggers (spicy food, caffeine, alcohol), and exercising regularly-also help significantly. These options carry fewer risks than hormone therapy and can be used long-term.
How often should I have my medications reviewed?
You should have a full medication review at least once a year. But you should also request one after any hospital stay, when you start or stop any medication, or when you see a new doctor. If you’ve been prescribed two or more new drugs in a short time, that’s a red flag. Bring your brown bag of all medications-prescription, over-the-counter, and supplements-to every appointment. This helps your doctor spot duplicates, interactions, and unnecessary drugs. Many Medicare Part D beneficiaries are eligible for free annual medication therapy management sessions with their pharmacist.



Man, this post hit home. I watched my mom go from 8 meds to 3 after her med review last year. She went from stumbling in the kitchen to dancing with her grandkids again. Transdermal patch for estrogen? Game changer. And ditching that damn diazepam? She sleeps better now without the brain fog.
Also, brown bag method? DO IT. I brought her whole medicine cabinet to her PCP last time - turned out she was getting the same BP med from two different docs. Classic polypharmacy trap.
Also, CBT for hot flashes? I didn’t know that was a thing. Now I’m sending this to every woman I know over 60. 🙌
Interesting breakdown, but let’s not oversimplify the pharmacokinetics. Hepatic first-pass metabolism isn’t just ‘slowed’-it’s CYP450 isoform downregulation, especially CYP3A4 and CYP2C9, which directly impacts statin and NSAID clearance. Also, renal GFR declines ~1% per year post-50, so renally excreted drugs like metformin and ACEis need dose adjustments based on eGFR, not just age.
And the Beers Criteria? Solid, but it’s not gospel. Some ‘inappropriate’ meds are still indicated for frail elderly with specific comorbidities. Context matters. Also, why no mention of deprescribing algorithms like STOPP/START? That’s the real clinical tool.
Also, tibolone’s stroke risk? 58% relative increase? That’s from the STARS trial, yes-but absolute risk is still <1% per year. Don’t scare people off with relative stats.
I’m a nurse practitioner and I see this every day. But honestly? Most patients don’t even know what they’re taking. One woman came in with 14 bottles and said, ‘I think this blue one is for my heart?’
And the doctors? They’re overworked. No one has time to do a full med review unless you push for it. You have to be the squeaky wheel. Bring the brown bag. Say, ‘I’m worried I’m on too much.’
Also, did you know some pharmacies now do automated med reconciliation? Ask your pharmacist. They’re the unsung heroes here.
This is powerful. In Nigeria, many older women take herbs with their pills because they think ‘natural = safe.’ But we have cases where bitter leaf tea messed with warfarin and caused bleeding. Or ginger with blood pressure meds-lowers it too much.
Thank you for saying this clearly. We need more of this kind of info in Africa too. 🙏
Well-researched, thoughtful, and urgently needed. I appreciate the specificity around transdermal vs. oral estrogen-this is precisely the nuance missing from mainstream media. Also, the emphasis on deprescribing as a clinical skill-not an afterthought-is refreshing.
That said: why no mention of the 2023 ACOG update on HRT duration? They now suggest, in low-risk women, up to 15 years may be acceptable if symptoms persist and no contraindications exist.
Also, the phrase ‘not harmless just because they’re natural’-brilliant. I’ve seen too many patients on high-dose black cohosh thinking it’s ‘just a supplement.’
Well done. 👏
Of course the pharmaceutical industry doesn’t want you to stop taking pills. They make billions off polypharmacy. And now they’re pushing ‘non-hormonal alternatives’-which are just antidepressants repackaged as ‘menopause solutions.’
Meanwhile, real hormone therapy is demonized because Big Pharma doesn’t own the patent on estrogen patches anymore. But the truth? Estrogen is life-saving for many women. They just don’t want you to know that.
And why are they so scared of tibolone? Because it’s cheap. And it works. 🤔
While the general thrust of this post is not without merit, it suffers from significant methodological and terminological imprecision. The phrase ‘liver metabolism slows’ is a gross oversimplification; hepatic clearance is not uniformly reduced but rather isoform-specific. Moreover, the assertion that ‘transdermal estrogen eliminates clotting risk’ is demonstrably false-it reduces risk relative to oral, but does not eliminate it.
Furthermore, the reference to the Women’s Health Initiative is cited without acknowledging the heterogeneity of the cohort (e.g., average age 63, many >10 years post-menopause). Modern guidelines (NAMS 2022) differentiate between early vs. late initiation.
Also, the Beers Criteria are not regulatory-they are a guideline. Misapplication leads to undertreatment.
Finally, the claim that ‘CBT reduces hot flashes as much as low-dose hormones’ is based on a single RCT with small n and subjective endpoints. Replication is limited.
Clarity is vital, but so is precision.
THIS IS A GOVERNMENT PLOT. They want you to stop estrogen because they’re trying to make women weak and dependent on antidepressants. The FDA is controlled by Big Pharma. They don’t want you to know estrogen prevents dementia, heart disease, AND keeps your skin young.
They call it ‘increased cancer risk’-but what about all the women who got cancer after taking those fake ‘non-hormonal’ SSRIs? Who’s studying that?
And why are they pushing ‘cooling techniques’? Because they don’t want you to be comfortable. They want you to suffer so you’ll take more pills.
Wake up. 🚨🇺🇸
Yo, I’m from the South and my grandma took five pills a day till she was 82. Then she started walking every morning, switched to a patch, and dropped three meds. Now she’s gardening, playing bingo, and telling everyone about it.
Don’t let doctors scare you. But don’t be dumb either. Talk. Ask. Bring the bag. And if you’re still feeling like crap after 6 months on paroxetine? Maybe it’s time to try something else.
And yeah-black cohosh? Yeah, it’s ‘natural.’ But so’s poison ivy. Don’t be fooled.