QT Prolongation Risk Calculator
This interactive tool helps you assess your risk for Torsades de Pointes (TdP), a potentially deadly heart rhythm caused by QT-prolonging medications. Based on the latest medical guidelines and risk factors from the CredibleMeds database.
Torsades de Pointes isn’t just another arrhythmia. It’s a heart rhythm that twists on the ECG like a snake, and it can kill you in seconds - often without warning. It doesn’t come from stress or exercise. It comes from medications you might be taking right now. And the scary part? You won’t feel it coming.
Every year, about 4 out of every million women and 2.5 out of every million men experience this rare but deadly reaction. Most don’t have symptoms until it’s too late. No chest pain. No dizziness. Just sudden collapse - or worse. But here’s the good news: this isn’t random. It’s predictable. And it’s preventable.
What Exactly Is Torsades de Pointes?
Torsades de Pointes (TdP) is a type of irregular heartbeat that shows up on an ECG as a wave that seems to twist around the baseline. The name comes from French - "twisting of the points" - and it’s unmistakable once you’ve seen it. But you won’t see it unless your QT interval is already too long.
The QT interval measures how long it takes your heart’s ventricles to recharge between beats. When that time stretches too far - past 500 milliseconds - your heart becomes electrically unstable. That’s when early, abnormal electrical signals (called afterdepolarizations) trigger the twisting rhythm of TdP. It can stop on its own, or it can turn into ventricular fibrillation - a chaotic, fatal rhythm.
Most cases happen because a drug blocks a specific potassium channel in your heart called hERG. This slows down the heart’s recovery phase, lengthening the QT interval. It’s not magic. It’s biology. And hundreds of common medications do exactly this.
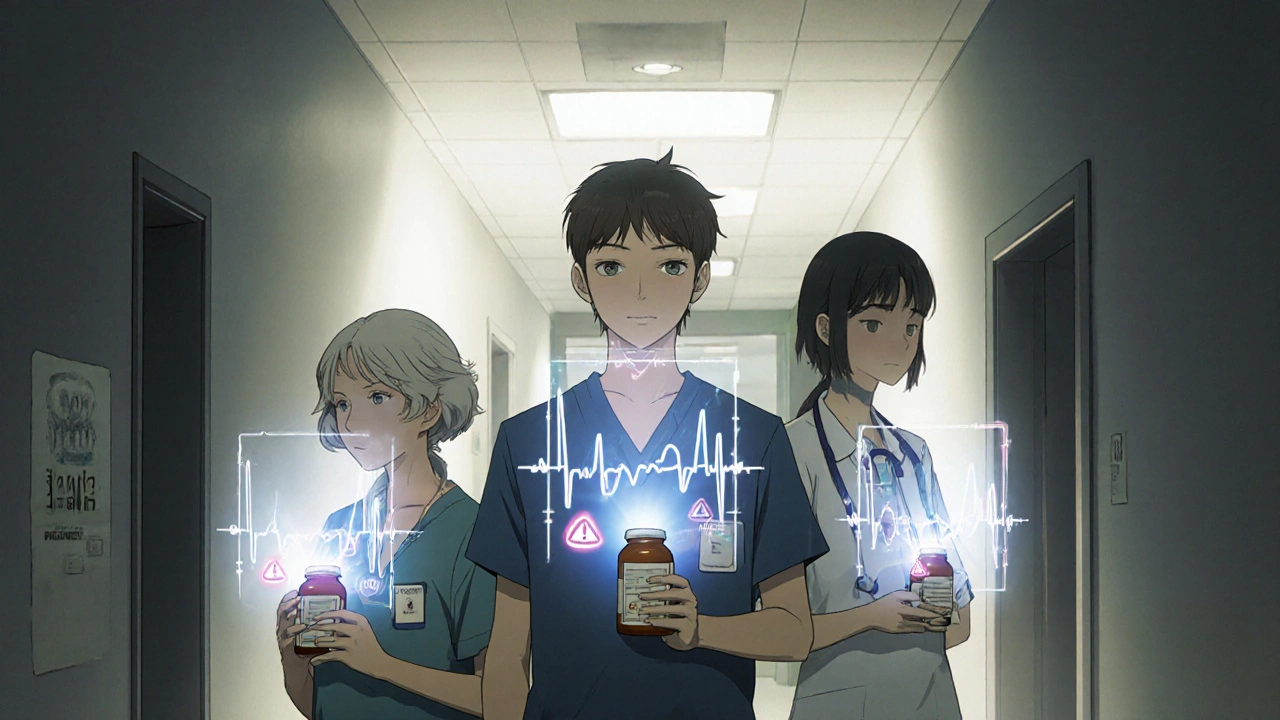
Which Medications Cause QT Prolongation?
You might be surprised how many everyday drugs can trigger this. It’s not just the ones you’d expect.
- Antibiotics: Erythromycin, clarithromycin, moxifloxacin
- Antifungals: Ketoconazole, voriconazole
- Antipsychotics: Haloperidol, thioridazine, ziprasidone
- Antidepressants: Citalopram, escitalopram (especially over 20 mg/day)
- Anti-nausea drugs: Ondansetron, dolasetron (especially IV doses over 16 mg)
- Pain meds: Methadone (risk spikes above 100 mg/day)
- Antiarrhythmics: Quinidine, sotalol, dofetilide - yes, drugs meant to fix heart rhythms can cause them
The CredibleMeds database classifies these drugs into three risk levels: "Known Risk," "Possible Risk," and "Conditional Risk." The difference matters. A drug in the "Known Risk" category has been directly linked to multiple TdP cases. A "Conditional" one only becomes dangerous if you’re also low on potassium or have kidney problems.
Some drugs were pulled from the market entirely - like terfenadine (Seldane) and cisapride (Propulsid) - because too many people died. Others carry black box warnings, the FDA’s strongest alert. Citalopram, haloperidol, and methadone all have them.
Who’s Most at Risk?
Not everyone who takes a QT-prolonging drug gets TdP. But certain people are sitting on a ticking time bomb.
- Women: 70% of all TdP cases occur in women, even though men and women have similar QT prolongation rates. Why? Hormones, body size, and slower drug metabolism play a role.
- People over 65: Two-thirds of cases happen in older adults. Kidneys and liver don’t clear drugs as well. Doses that were safe at 40 become dangerous at 70.
- Low potassium or magnesium: If your potassium is below 3.5 mmol/L, your risk triples. Below 1.6 mg/dL for magnesium? Risk jumps 2.7 times. These are easy fixes - but often overlooked.
- Heart disease: If you’ve had a heart attack, heart failure, or a prior arrhythmia, your heart is already vulnerable.
- Multiple QT drugs: Taking two or more QT-prolonging meds at once increases risk by nearly 30%. It’s not additive - it’s explosive.
- Slow heart rate: Bradycardia (under 60 bpm) gives the heart more time to develop dangerous electrical activity.
- Genetics: People with inherited long QT syndrome (even mild forms) are at extreme risk. About 1 in 2,000 people carry a hidden mutation.
One study found that 87% of TdP patients had at least one of these risk factors - and most were already known to their doctors. The problem wasn’t ignorance. It was inaction.
How to Prevent It Before It Starts
Prevention isn’t complicated. It’s systematic. Here’s the 5-step plan used by top cardiac safety teams:
- Screen for inherited long QT: Use the Schwartz score - a simple checklist of symptoms like fainting, family history, and ECG changes. If you’ve had unexplained fainting before age 40, get tested.
- Check your electrolytes: Get a blood test for potassium and magnesium before starting any high-risk drug. If you’re low, fix it. Don’t wait.
- Review every medication: Go to CredibleMeds.org and search every pill you take. Even over-the-counter ones. Some antihistamines and herbal supplements can prolong QT too.
- Get a baseline ECG: Before starting methadone, citalopram, or any high-risk drug, get an ECG. Measure your QTc. If it’s over 450 in men or 460 in women, you’re already in a caution zone.
- Set a monitoring plan: For methadone, repeat ECGs at 100 mg/day. For citalopram, don’t go over 20 mg if you’re over 60. For ondansetron, avoid IV doses over 16 mg. Stick to the rules.
VA Healthcare data showed that following this protocol reduced TdP cases by 78% over four years. That’s not luck. That’s discipline.
What to Do If TdP Happens
If someone collapses and you suspect TdP - don’t wait. Call 911. Start CPR if they’re unresponsive.
In the hospital, treatment is fast and specific:
- Magnesium sulfate: Give 1-2 grams IV immediately. It works in 82% of cases, even if magnesium levels are normal. It’s the first-line treatment.
- Temporary pacing: Speed up the heart rate to over 90 bpm. This shortens the QT interval and stops the twisting rhythm. It works in 76% of cases.
- Correct electrolytes: Raise potassium to above 4.0 mmol/L and magnesium to above 2.0 mg/dL.
- Isoproterenol: If pacing isn’t available, this drug can increase heart rate and stabilize the rhythm.
- Stop the drug: Immediately discontinue the QT-prolonging medication.
Defibrillation is used if TdP turns into ventricular fibrillation - but it’s a last resort. Prevention is far better than emergency response.
The Bigger Picture: Why This Matters
Drug companies now spend over $1 million extra and 6-8 months longer testing every new drug for QT effects. The FDA requires it. Why? Because of deaths. Terfenadine killed 125 people before it was pulled. Cisapride killed dozens more.
Today, the FDA no longer demands blanket avoidance of QT-prolonging drugs. They want smart use. A drug like methadone saves lives in addiction treatment. Citalopram helps people with depression. The goal isn’t to ban them - it’s to use them safely.
That’s why the 2022 PREVENT TdP Act was introduced. It pushes for standardized ECG monitoring across hospitals and clinics. If passed, it could prevent 200 deaths a year.
And new tools are coming. Mayo Clinic’s machine learning model now predicts individual TdP risk with 89% accuracy by analyzing 17 factors - age, sex, meds, kidney function, ECG trends. Personalized risk assessment is no longer science fiction.
Final Takeaway
Torsades de Pointes is rare. But it’s not mysterious. It’s not inevitable. It’s a known consequence of known actions - and known inactions.
If you’re prescribed a drug that prolongs QT, ask: "Do I have any risk factors? Have I had my QT checked? Am I on other drugs that could make this worse?" If you’re a clinician, don’t assume your patient’s potassium is fine. Check it. Don’t assume they’re not on another QT drug. Ask them. Review their list.
The next time you or someone you care about starts a new medication, don’t just take it. Understand it. And if you’re unsure, get an ECG. One simple test can save a life.



So let me get this straight - we’re now supposed to get an ECG before taking ibuprofen? Next they’ll make us scan our blood for alien parasites. This is medical gaslighting dressed up as ‘safety.’
i just took citalopram for 3 years and never even knew my qt was long until my mom had a scare and we looked it up. i’m 52, female, on a low dose, and my doc never mentioned it. why? because they’re overworked and underpaid and honestly? we’re just numbers in a system that’s too broken to care. but this post? this actually saved me. thank you.
It’s frankly irresponsible that pharmaceutical companies are allowed to market drugs with such well-documented lethal potential without mandatory ECG screening for all patients. The fact that this isn’t standard protocol in every primary care office is a moral failure of the medical-industrial complex. People die because we prioritize convenience over caution - and those who do are conveniently labeled ‘unfortunate outliers.’
Wait - so ondansetron can cause this? I got that IV after my surgery last month. Should I be worried? I didn’t know anything about QT intervals before this. I just thought it was for nausea.
Interesting how the West obsesses over QT prolongation while ignoring the fact that 80% of global populations have no access to basic ECG machines. This is elite medicine for the privileged. Meanwhile, in India, people die from sepsis because they can’t afford antibiotics - but we’re all supposed to panic about a 0.0004% risk? Colonial thinking in a white lab coat.
You know what’s really dangerous? Trusting a system that profits off your fear. They scare you with TdP so you’ll take more tests, more meds, more follow-ups - all while the real killers - poverty, stress, pollution - go unaddressed. This isn’t medicine. It’s monetized anxiety.
Thank you for writing this. I’m a nurse and I’ve seen two TdP cases. One was a 68-year-old woman on methadone and citalopram with a potassium of 3.1. She survived because her ECG was done before discharge. The other? She didn’t get screened. She didn’t make it. This isn’t theoretical. It’s real. Please, if you’re on any of these meds - ask for the ECG. It takes 5 minutes. It could save your life. ❤️
One cannot help but observe the absurdity of a pharmacopeia that has, over the last three decades, systematically weaponized the very mechanisms designed to heal. We have turned cardiac electrophysiology into a high-stakes game of Russian roulette - and the house always wins, because the house is Big Pharma. The FDA’s ‘black box’ warnings? A performative gesture. A fig leaf. A bureaucratic tick-box. We are not being protected. We are being managed.
My grandma died from this. She was on Zoloft and a Z-Pack. No one told her. No one asked if she was on anything else. She was 74. She went to bed fine. Woke up dead. I’ve spent 7 years screaming into the void about this. Nobody listens until it’s their mom. Or their dad. Or their sister. Now I just hand people this post. No words. Just this. And they cry. And then they get tested.
Thank you for this meticulously researched and profoundly compassionate exposition. The integration of clinical data, actionable protocols, and humanistic urgency is a model for medical communication. I have shared this with my entire care team and will advocate for institutional adoption of the 5-step prevention framework. 🙏
Let’s not ignore the elephant in the room: this entire panic is engineered. The FDA, WHO, and AMA are pushing this narrative to justify the expansion of surveillance medicine. Who benefits? The ECG machine manufacturers. The labs. The data brokers. You think they want you healthy? No. They want you monitored. Always. This is the beginning of mandatory cardiac tracking for all prescription users. Wake up.
Okay but what about the fact that in India, we have patients on 10 different QT-prolonging drugs because they can’t afford specialists? We don’t have ECGs in rural clinics. We don’t even have potassium tests. So we just hope. And sometimes, people die. But you know what? We don’t have the luxury of 5-step protocols. We have one step: survive today. This post is beautiful. But it’s written for people who can afford to be careful. The rest of us? We’re just trying to live.
This is the kind of post that makes me believe in humanity again. You didn’t just list facts - you gave people power. I’m a pharmacy tech and I’m going to start asking every patient: ‘Are you on anything that might affect your heart?’ It’s simple. It’s free. It’s everything. Thank you for seeing us. 💛
I’ve been on escitalopram for 8 years. My doctor never mentioned QT. I’m 58, post-menopausal, and my potassium was always ‘normal.’ But now I’m getting my ECG next week. Not because I’m scared - because I’m grateful. Knowledge isn’t fear. It’s freedom. And you gave me that.
I read this and just cried. My brother died from TdP at 42. He was on methadone for chronic pain and took an OTC antihistamine for allergies. No one told him. No one asked. He was just ‘a healthy guy.’ This is the quiet epidemic. And now I’m telling everyone I know.