When you take a pill, get a shot, or rub on a cream, you’re not just choosing how to take your medicine-you’re choosing what kind of side effects you might face. It’s not just about convenience or fear of needles. The way a drug enters your body changes everything: how fast it works, how much of it actually gets into your system, and what kind of trouble it might cause along the way.
Oral: The Easy Choice With Hidden Risks
More than 75% of all medications are taken by mouth. It’s simple: swallow a pill, wait a bit, and hope it works. But that simplicity comes with trade-offs. When you take a drug orally, it has to survive your stomach acid, get absorbed through your gut, and then pass through your liver before it ever reaches your bloodstream. That’s called first-pass metabolism, and it knocks out a big chunk of the drug before it can do its job.
For example, propranolol, a common heart medication, only has about 25% bioavailability when taken by mouth. That means you need to take a much higher dose than if it were injected directly. Higher dose? That means more chances for side effects. About 25-30% of people on oral NSAIDs like ibuprofen or naproxen end up with stomach upset. And for long-term users, 1-2% develop ulcers. It’s not rare-it’s expected.
Food makes it worse. Around 40% of common oral medications interact with meals. Taking a blood pressure pill with grapefruit juice? That can spike levels dangerously. Taking antibiotics on a full stomach? Might not absorb at all. These aren’t edge cases-they’re everyday problems.
And yet, people still prefer it. In one study, 92% of patients chose oral over injection if both worked the same. Why? Because it’s quiet, it’s private, and you don’t need help. But that ease leads to misuse. One in four antibiotic courses are taken incorrectly because people feel better after a few days and stop early. That’s how superbugs grow.
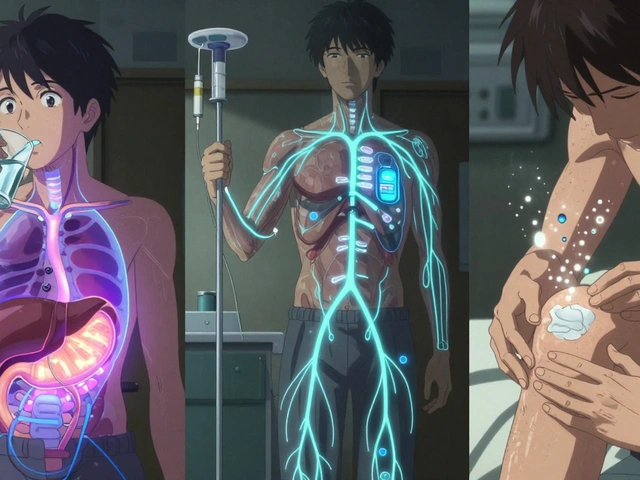
Injection: Fast, Precise, But Not Risk-Free
Needles scare people. About 20-25% of adults have needle phobia. But for some drugs, there’s no alternative. If you’re having a heart attack, waiting 60 minutes for a pill to kick in isn’t an option. Intravenous drugs hit your bloodstream in under five minutes. That’s why emergency rooms use injections for pain, seizures, infections, and cardiac arrest.
Injectables bypass the liver entirely. That means 100% of the drug gets into your system. That’s great for effectiveness-but dangerous if the dose is wrong. A small miscalculation in an IV drip can cause a crash in blood pressure or an overdose. That’s why they’re given by trained staff in hospitals.
Even when patients self-inject-like with insulin or biologics for arthritis-the risks don’t disappear. Injection site reactions happen in 15-20% of cases. Redness, swelling, bruising. For diabetics on long-term insulin, 45% develop lumps under the skin called lipohypertrophy. That’s where fat builds up from repeated injections in the same spot, and it makes insulin absorption unpredictable.
And then there’s cost. A single dose of a biologic injectable for rheumatoid arthritis can cost $2,500-$5,000. The oral version? $25-$100. That’s why 28% of patients on injectables skip doses or stop altogether. Cost isn’t just a number-it’s a barrier to health.
Needle disposal is another hidden problem. Forty percent of people don’t have access to proper sharps containers. Some throw needles in the trash. Others flush them. That’s not just irresponsible-it’s dangerous for sanitation workers and kids.
Topical: Localized Relief, Minimal Systemic Trouble
Put a cream on your knee for arthritis. Apply a patch for nicotine withdrawal. Rub steroid ointment on eczema. These are all topical routes-and they’re designed to stay local. That’s the key. When a drug doesn’t enter your bloodstream, it doesn’t cause the same kind of side effects as pills or shots.
Topical corticosteroids for skin conditions show 92% less suppression of the HPA axis (a major hormone system) than oral versions. That’s huge. Oral steroids can cause weight gain, mood swings, high blood sugar, and bone loss. Topical? Almost none of that-if used correctly.
Transdermal patches, like those for pain or nicotine, are a special case. They’re designed to slowly leak drugs through the skin into the blood. But even then, systemic exposure is far lower than with pills. A fentanyl patch delivers steady pain relief without the spikes and crashes you get with oral opioids. That’s why 74% of chronic pain patients in one Mayo Clinic survey preferred patches.
But topical doesn’t mean foolproof. Skin isn’t a uniform barrier. If you have psoriasis or damaged skin, your body absorbs 3-5 times more drug than normal. That’s why some people get unexpected side effects from topical steroids-even though they were told it’s “safe.”
And application matters. Most people use too little. A fingertip unit (the amount of ointment from the tip of your finger to the first crease) is the standard dose for skin creams. But studies show 60% of patients apply less than half that. Result? The treatment doesn’t work. They think it’s ineffective. So they double up. And then they get thin skin, stretch marks, or even adrenal suppression.
Topical delivery also has physical limits. Only small molecules-under 500 Daltons-can sneak through skin. That’s why insulin, vaccines, and most biologics can’t be delivered this way… yet. But new tech is changing that. Ultrasound-enhanced patches introduced in 2023 can push large molecules through skin 600% better than old patches. Soon, we might see biologics delivered without needles.

What’s the Best Choice?
There’s no universal winner. Each route has its place.
Choose oral for long-term, stable conditions where speed isn’t critical-like high blood pressure, cholesterol, or thyroid meds. But be honest about the stomach issues and interactions. Don’t assume it’s harmless.
Choose injection when you need fast action, precise dosing, or your gut can’t absorb the drug-like in severe infections, diabetes, or autoimmune flare-ups. But prepare for cost, training, and injection site problems.
Choose topical for skin, joint, or localized pain issues. It’s the safest route for avoiding systemic side effects. But use the right amount. Apply it correctly. And don’t assume it’s risk-free just because it’s on the outside.
Doctors don’t pick routes randomly. They weigh speed, safety, cost, and your lifestyle. If you’re on a pill that gives you nausea every day, ask: Could a patch help? If you’re terrified of needles but your insulin dose keeps changing, ask: Is there an oral alternative in development? If you’re using a cream that doesn’t seem to work, ask: Am I using enough?
Medicine isn’t just about what you take. It’s about how you take it.
Real-World Trade-Offs
Here’s how the three compare in practice:
| Factor | Oral | Injection | Topical |
|---|---|---|---|
| Onset of Action | 30-90 minutes | 2-5 min (IV), 45-90 min (IM/SC) | 15 min-24 hours (depends on formulation) |
| Bioavailability | 5-100% (often low due to first-pass) | 70-100% (no first-pass) | 5-80% (mostly local; 60-80% for transdermal) |
| Common Side Effects | Stomach upset, nausea, ulcers, drug interactions | Infection, pain, lipohypertrophy, anaphylaxis | Skin irritation, dryness, rare systemic effects |
| Systemic Exposure | High | Very high | Low (unless transdermal) |
| Cost (Average per Dose) | $25-$100 | $250-$5,000 | $30-$150 |
| Patient Preference | 92% prefer if equally effective | 20-25% avoid due to needle fear | 68% prefer for skin conditions |
| Self-Administration | 95% can do it correctly | 60-70% need training | 60% apply incorrectly |
The bottom line? The route isn’t just a detail-it’s part of the treatment. A pill might be cheaper, but if it ruins your stomach, you’re not saving money-you’re trading one problem for another. An injection might be faster, but if you skip it because you hate needles, you’re not getting better. A cream might seem safe, but if you use too little, you’re wasting your time.

What’s Next?
The future of drug delivery is moving away from one-size-fits-all. New oral technologies-like liquid-in-capsule systems-are boosting absorption for drugs that used to fail in the gut. Auto-injectors with real-time feedback are making self-injection safer. And ultrasound patches could one day replace insulin shots entirely.
But until then, the best choice depends on your body, your condition, and your life. If you’re struggling with side effects from your current route, talk to your doctor. Don’t just live with nausea. Don’t just dread the needle. Don’t just guess how much cream to use. Ask: Is there another way?
Which route has the fewest side effects?
Topical administration generally has the fewest systemic side effects because it’s designed to act locally. For example, topical steroids for eczema cause far less hormone disruption than oral steroids. However, if the product is misused-applied too often or on broken skin-it can still cause problems. Injectable routes have higher risks of infection and allergic reactions, while oral routes commonly cause nausea, ulcers, and drug interactions. So while topical wins for safety, proper use is critical.
Can I switch from oral to topical for my condition?
It depends on the drug and the condition. For skin issues like eczema, psoriasis, or joint pain, switching to a topical form is often possible and recommended. For systemic conditions like high blood pressure or depression, oral or injectable routes are usually necessary because topical forms can’t deliver enough drug into the bloodstream. Always consult your doctor before switching-some medications simply can’t be delivered through the skin.
Why do some pills make me sick but injections don’t?
Because oral drugs pass through your stomach and liver before entering your bloodstream. That process can irritate your gut lining and break down the drug, forcing your body to handle higher doses to get the same effect. Injections skip this step-they go straight into your blood. So if you get nausea or stomach pain from pills but not shots, it’s likely because your GI tract is reacting to the drug’s passage, not the drug itself.
Are transdermal patches safer than pills?
For many drugs, yes. Patches like those for pain or nicotine deliver medication slowly and steadily, avoiding the peaks and crashes that cause side effects with pills. They also reduce liver exposure, lowering the risk of liver toxicity. But patches aren’t risk-free-they can cause skin irritation, and if you sweat a lot or shower too soon after applying, the dose can be inconsistent. Still, for chronic conditions, they’re often safer than daily pills.
Why can’t all drugs be given as a pill?
Some drugs are too large (like proteins in biologics), too unstable in stomach acid, or too poorly absorbed by the gut. Others are destroyed by liver enzymes before they ever reach the bloodstream. That’s why insulin, vaccines, and many cancer drugs must be injected. Researchers are working on oral versions, but for now, science still needs needles for certain treatments.
How do I know if I’m using my topical cream correctly?
Use the fingertip unit rule: squeeze out a line of cream from the tube to the first crease of your index finger. That’s one unit. One unit covers an area about the size of two adult hands. Apply it gently, once or twice a day as directed. Don’t rub it in hard. Don’t use more because you think it’ll work faster. If your skin doesn’t improve in 1-2 weeks, talk to your doctor-you might need a stronger formulation or a different route.
Is it safe to use expired topical creams?
No. Topical products can degrade, lose potency, or even grow bacteria after their expiration date. Steroid creams, for example, may stop working, forcing you to overapply-which increases the risk of skin thinning. Antibiotic creams can become ineffective, leading to resistant infections. Always check the expiration date and discard any cream that smells off, changed color, or separated.
Final Thought
Your body doesn’t care if a drug is called ‘strong’ or ‘new.’ It only responds to how it gets in. A pill might be easy, but it’s not always the safest. A shot might be scary, but it might be the only way to get real relief. A cream might seem weak, but if used right, it could be the most powerful tool you have. The route isn’t just a delivery method-it’s part of the medicine itself.


8 Comments
Write a comment