When you pick up a prescription, you might not notice the difference between the brand-name pill and the generic one. Same active ingredient. Same dosage. Same color, sometimes even the same shape. But if you ask patients how they feel about it - generic medications - the answer isn’t always straightforward.
It’s Not About the Drug, It’s About the Mind
People don’t judge medications the way they judge smartphones or coffee. You don’t open a pill bottle and taste-test the chemistry. You feel it. You notice if your headache doesn’t go away. If your blood pressure feels off. If you get a stomach ache where you didn’t before. And when that happens, even if science says it’s the same drug, your brain says otherwise. This is brand psychology in action. The name on the bottle - whether it’s Lipitor or lisinopril - triggers expectations. A 2024 study in Nature Communications found that 72% of patients reported dissatisfaction with at least one generic medication, not because it didn’t work, but because they believed it wouldn’t. The drug didn’t change. Their perception did. In Australia, where generics make up over 85% of prescriptions, that gap between expectation and reality is still wide. Patients who’ve been on a brand-name drug for years often feel like they’re being handed a knockoff. Even when the pharmacy tells them it’s bioequivalent - meaning it delivers the same amount of medicine into the bloodstream within the same timeframe - the word ‘generic’ carries weight. It sounds cheaper. Less reliable. Less cared-for.What Actually Drives Satisfaction?
Research using the Generic Drug Satisfaction Questionnaire (GDSQ) breaks patient satisfaction into three clear parts: effectiveness, convenience, and side effects. And guess what? Effectiveness tops the list. A 2021 study published in Sage Publications found that how well patients believe the drug works accounts for 25.4% of their overall satisfaction score. Convenience - things like pill size, frequency of dosing, or how easy it is to refill - adds another 23.7%. Side effects? They’re the loudest. Five out of twelve GDSQ questions focus on them. One patient might say, “My generic statin made me feel weak.” Another says, “It’s the same as before, but cheaper.” Same drug. Different stories. The data doesn’t lie: for antibiotics, satisfaction hits 85.3%. For antiepileptics? Only 68.9%. Why? Because with drugs that control seizures, heart rhythms, or thyroid levels, even tiny changes in blood concentration can feel like a crisis. Patients aren’t being irrational - they’re reacting to real experiences, even if those experiences aren’t caused by the drug itself.Doctors and Pharmacists Are the Missing Link
Here’s the surprising part: when a doctor or pharmacist explains what’s happening, satisfaction jumps. A 2023 study in PLOS ONE showed that when Australian GPs took just three minutes to explain that generics must meet the same FDA and TGA standards - including a strict 80-125% bioequivalence range - patient satisfaction rose by 34.2%. That’s not magic. That’s communication. Patients aren’t angry because generics are cheaper. They’re angry because they weren’t told the truth. They were handed a new pill with no context. No reassurance. No explanation that the FDA requires generics to perform identically to brand-name drugs in 90% of cases. In Greece, where doctors actively promote generics, 69.8% of patients said they’d accept them if recommended. In Saudi Arabia, where information is scarcer, only 45% believed generics were as effective as international brands. The difference? Trust. And trust comes from the person handing you the script.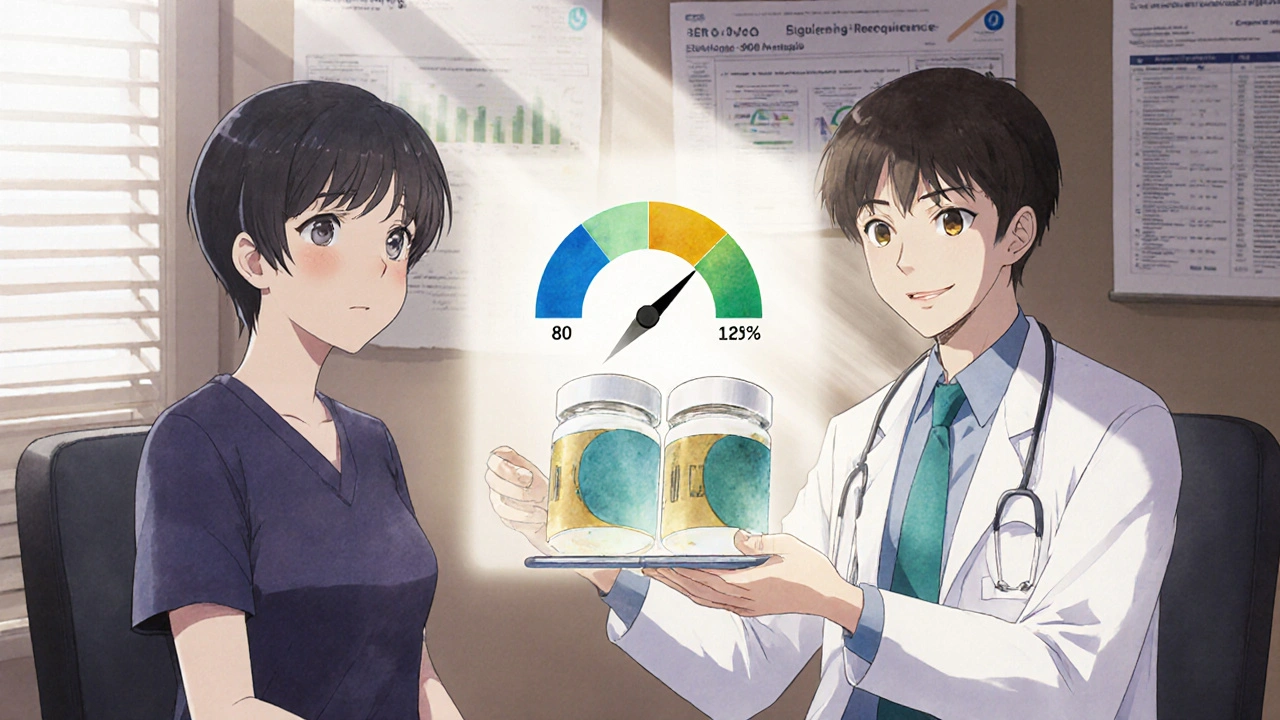
Cost Matters - But Not the Way You Think
Yes, generics save money. In the U.S., they cut prescription costs by 80-90%. Globally, the generic drug market hit $475.8 billion in 2023. But cost isn’t the main driver of satisfaction. Patients who switched from brand-name Synthroid to generic levothyroxine and saw their TSH levels go haywire didn’t care about the $35 price drop. They cared about their body feeling wrong. On the flip side, someone switching from Prinivil to lisinopril and saving $36 a month might say, “It works exactly the same.” The real win? When cost enables adherence. A patient on a fixed income might skip their blood pressure pill if it costs $40. Switch to the $4 generic? They take it every day. That’s not satisfaction - that’s survival. And it’s why satisfaction scores rise when affordability removes barriers.Why Some Drugs Trigger More Doubt
Not all generics are treated the same. Antidepressants and antiepileptics are the most complained-about. Why? Because these drugs affect the brain. And the brain is sensitive. Even a 5% variation in blood levels - well within the legal bioequivalence range - can feel like a crash. Reddit threads from 2023-2024 show that 32.1% of negative comments about generics involve antidepressants. One user wrote: “I was stable on brand-name sertraline. Switched to generic. Felt like I was falling apart. Went back. Now I’m fine.” It’s not that the generic is worse. It’s that the brain interprets change as danger. Especially when you’re already fragile. Meanwhile, antibiotics? 85% satisfaction. Why? Because the effect is fast. You take it, you feel better in two days. No room for doubt. No time for anxiety to creep in.The Measurement Problem
We measure patient satisfaction with surveys, questionnaires, and interviews. But these tools were mostly designed in the U.S. and Europe. They don’t always translate. A 2020 study in the Journal of Cross-Cultural Psychology found that patients in collectivist cultures - like Japan or Saudi Arabia - report satisfaction scores 32% higher than those in individualist cultures, even when outcomes are identical. Why? Because in collectivist societies, trusting authority figures - doctors, pharmacists - is part of the culture. Questioning the drug? That’s seen as disruptive. And then there’s the Hawthorne effect: when patients know they’re being studied, they report higher satisfaction. One study found this inflated scores by 18.7%. So if a pharmacy surveys you right after you get your prescription, you’re more likely to say “it’s fine” - even if you’re skeptical. The real challenge? We’re measuring perception, not pharmacology. And perception is messy.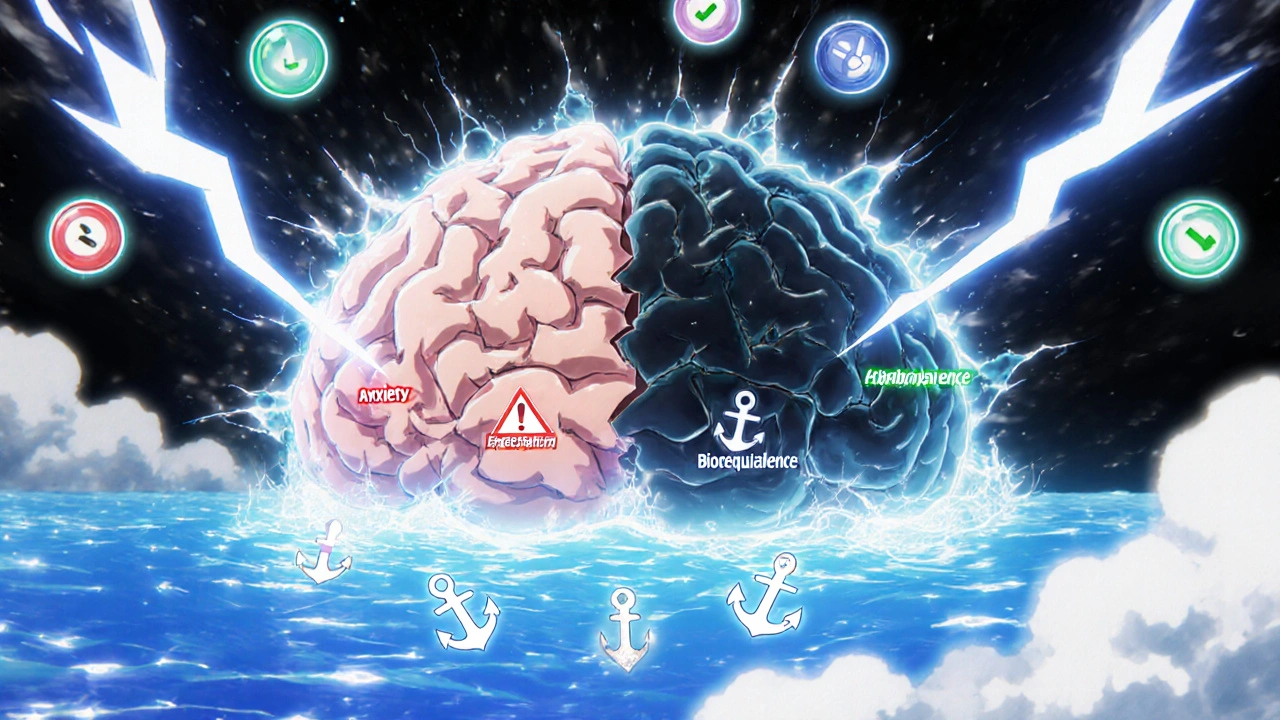
What’s Changing - and What’s Next
The FDA launched its Generic Drug User Fee Amendments (GDUFA) III Patient Perception Initiative in 2024, pouring $15.7 million into better ways to measure how patients really feel. Meanwhile, the European Commission is analyzing half a million social media posts across 28 languages to map how people talk about generics online. The future? Personalized satisfaction tracking. Mayo Clinic is testing a pilot where genetic testing helps predict how a patient might respond to a generic drug. If your genes make you a slow metabolizer of certain medications, you might need a different formulation - brand or generic. This isn’t science fiction. It’s happening now. And it’s not about choosing between brand and generic. It’s about choosing the right tool for the right person.What Patients Need to Know
If you’ve been switched to a generic and feel off:- Don’t assume it’s the drug. Talk to your doctor or pharmacist. Ask: “Could this be a change in fillers or coating? Is this bioequivalent?”
- Keep a simple journal: note when you take it, how you feel, any side effects. Patterns matter more than one bad day.
- Ask if you can try the brand again - even temporarily - to compare. Sometimes, it’s not the drug. It’s the transition.
- Remember: generics are required to be just as safe and effective. But your experience matters too. If something feels wrong, it’s worth investigating.
What Providers Need to Do
Doctors and pharmacists aren’t just dispensers. They’re translators.- Don’t say, “It’s the same.” Say, “This generic meets the same strict standards as the brand. The only difference is the inactive ingredients - and the price.”
- Explain bioequivalence. Use the 80-125% range. Make it real.
- For high-risk drugs - thyroid, epilepsy, blood thinners - offer to monitor levels after the switch.
- Don’t assume patients know the difference between efficacy and perception. Most don’t.
Generic medications aren’t second-rate. They’re a triumph of science and public policy. But until we fix the story we tell patients - until we stop treating satisfaction as a number and start treating it as a conversation - the gap between what’s true and what’s felt will stay wide.
Are generic medications really as effective as brand-name drugs?
Yes. By law, generic medications must contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet the same strict standards for bioequivalence - meaning they deliver the same amount of medicine into your bloodstream within the same timeframe, typically within an 80-125% range. Regulatory agencies like the FDA and TGA require this before approval. Studies show generics work just as well in 90% of cases. But perception often lags behind science.
Why do some people feel worse after switching to a generic?
The active ingredient is the same, but inactive ingredients - like fillers, dyes, or coatings - can differ. For most people, this makes no difference. But for those on narrow therapeutic index drugs - like thyroid meds, seizure drugs, or blood thinners - even small changes in how the drug is absorbed can cause noticeable effects. These aren’t always due to the generic itself. Sometimes, it’s the body adjusting to a new formulation after years on a brand. A doctor can check blood levels or temporarily switch back to confirm.
Do generics have more side effects?
No. The side effect profile of a generic must match the brand-name drug. Any differences reported are usually due to psychological factors - like expecting a problem - or changes in inactive ingredients that affect how the pill is absorbed. Rarely, a patient might react to a new filler (like lactose or gluten), but this is uncommon and can be tested. If you notice new side effects after switching, talk to your pharmacist. They can check if the formulation changed.
Can I ask for the brand-name drug instead?
Yes. In most countries, including Australia and the U.S., you can request the brand-name version. But your insurance may not cover it, or you may pay more out of pocket. If you have a medical reason - like a documented reaction to a specific generic - your doctor can write a “dispense as written” or “do not substitute” note. For most people, though, generics are safe, effective, and the best financial choice.
Why are generics cheaper if they’re the same?
Brands spend millions on research, marketing, and patents. Generics skip all that. Once a patent expires, multiple companies can make the same drug. Competition drives prices down. A brand-name drug might cost $40 because of advertising and R&D recovery. The generic costs $4 because it only needs to prove it works the same way - not reinvent the wheel. The savings go to patients and healthcare systems - not to the manufacturer’s ad budget.
Is there a way to tell if a generic is right for me?
Start with trust. Ask your doctor or pharmacist to explain why the switch is happening. For high-risk drugs, ask for a blood test before and after the switch to check levels. Keep a simple log of how you feel. If you notice a pattern - like fatigue or mood changes - bring it up. Most people adapt fine. But if you don’t, you have the right to try the brand again. Your experience matters as much as the data.


OMG YES this is SO TRUE 😭 I switched to generic levothyroxine and felt like I was drowning in fog for 3 weeks. My doctor said "it's the same" but my body knew better. Went back to brand-now I’m sleeping, not crying, and my hair isn’t falling out. 🙏 #GenericWoes
So let me get this straight-you’re telling me my brain is the problem, not the pill? Like, I’m just delusional because I *felt* worse after the switch? Classic. 😏 Meanwhile, my pharmacist handed me a new bottle with zero explanation, and now I’m Googling "can inactive ingredients cause anxiety" at 2 a.m. Thanks, healthcare system.
Hey I'm a pharmacist and I see this every day. The real issue isn't the drug-it's the handoff. Patients get a generic shoved in their hand like it's a coupon for cereal. No context. No "hey this might feel weird at first." We need to stop treating this like a transaction and start treating it like a conversation. Bioequivalence isn't magic-it's math. But people aren't math. They're scared. They're tired. They've been told for years that "brand means better." We need to meet them where they are. And yes, three minutes of talking can change everything. Seriously. Try it.
I switched from brand to generic for my blood pressure med. No difference. Took it same time every day. Same results. Cost me $4 instead of $40. Why is this even a debate? If it works, it works. Simple.
Oh wow, so the problem is that people are too emotional? That’s rich. Coming from a country where the average person spends 10% of their income on meds and still gets charged $30 for a 30-day supply of generic insulin? Maybe if your system didn’t treat patients like dollar signs, people wouldn’t feel like they’re being scammed. But hey, let’s just blame their "perception."
My cousin in Delhi takes generic antiepileptic and says it’s fine, but I read online that some generics in India have bad fillers. Should I be scared? I’m not sure what to believe anymore. Everyone says something different. I just want to not have seizures.
Oh my GOD. I can’t believe people still think generics are "the same"?? Like, come on. The pill looks different. The taste is weird. The packaging is trash. And you’re telling me it’s just "inactive ingredients"?? That’s like saying two BMWs are the same because they both have four wheels. 🤦♀️ I’m paying $40 for a reason. I’m not some peasant who needs a "budget" version of my life-saving drug.
in india we use generics all the time and most people are fine. but i think in usa people are used to fancy brands and think expensive = better. also, sometimes doctor dont explain. i had friend who switched to generic for depression and felt bad. he told doctor. doctor checked blood level. it was fine. it was just his mind. but doctor listened. that helped. trust matters.
Look, I’ve been on the same generic statin for six years. No issues. But I’ve also seen people freak out over a change in the pill’s shape or color-even when it’s the exact same dosage from the same manufacturer, just a different batch. The psychological component here is massive. It’s not just about the drug. It’s about control. When you’ve been on the same pill for a decade and suddenly it looks different, your brain goes into survival mode. You didn’t choose it. You didn’t approve it. And now your body is doing something weird. Of course you’re going to blame the pill. It’s not irrational. It’s human. We’re wired to associate change with threat. The fact that science says it’s safe doesn’t override that instinct. That’s why communication isn’t optional. It’s essential. And no, telling someone "it’s the same" doesn’t cut it anymore.
People are lazy. They don’t want to think. They want a magic pill that doesn’t change. If it’s cheaper, it’s inferior. That’s not science. That’s ignorance. And now we’re spending millions to fix a problem created by people who refuse to read a single sentence about bioequivalence.
So… the answer is… just trust your doctor? But what if your doctor doesn’t care? What if they’re just rushing through appointments? What if they’re the ones who switched you without telling you? Then what? You’re just supposed to sit there and feel like crap because science says you shouldn’t? That’s not a solution. That’s gaslighting with a stethoscope.