Drug Interaction: What You Need to Know to Stay Safe
When you take more than one medication, or even a supplement with your prescription, you’re risking a drug interaction, a reaction between two or more substances that changes how they work in your body. Also known as medication interaction, it’s not just about pills clashing—it’s about how food, herbs, and even your own body chemistry can turn a safe dose into a dangerous one. This isn’t theoretical. One in five adults over 65 takes five or more medications, and nearly half of them are at risk for a harmful interaction. It’s not about being careless—it’s about how complex modern medicine has become.
Polypharmacy, the use of multiple medications at once, is common, especially for people managing chronic conditions like diabetes, high blood pressure, or arthritis. But each added drug increases the chance of something going wrong. For example, taking a common painkiller like ibuprofen with blood pressure medicine can knock your kidneys out of balance. Or mixing antidepressants like MAOIs with tyramine-rich foods—aged cheese, cured meats, draft beer—can spike your blood pressure to life-threatening levels. Even something as simple as drinking grapefruit juice can stop your liver from breaking down statins, leaving too much in your system. These aren’t rare cases. They happen daily, often because no one asked the right questions. Then there’s food-drug interactions, how what you eat changes how your body absorbs or processes medicine. Levothyroxine, for instance, loses up to 50% of its effect if taken with protein shakes or calcium-rich foods. Gastrointestinal issues like acid reflux or Crohn’s disease can block absorption entirely, making your meds useless even if you take them perfectly. And don’t forget storage—keeping pills in a humid bathroom or near the stove can break them down before you even swallow them.
What makes this worse is that most people don’t know what they’re taking. A study found that nearly 40% of seniors couldn’t name all their meds, let alone explain why they were on them. That’s why medication safety, the practice of managing drugs to avoid harm isn’t just about following labels—it’s about asking, documenting, and double-checking. Did your cardiologist talk to your rheumatologist? Did your pharmacist know you started taking turmeric for joint pain? Did your doctor know you switched from brand to generic and now feel worse? These gaps are where drug interactions slip through.
That’s why the posts below cover real situations—not theory. You’ll find how to avoid duplicate prescriptions after specialist visits, why timing your protein shake matters with thyroid meds, how to safely taper off steroids without crashing, and what foods to skip if you’re on an MAOI. You’ll see how insurance deals and pharmacy pricing can make generics harder to use than they should be, and why some people feel worse switching to generics—not because of chemistry, but because of perception. This isn’t a list of warnings. It’s a practical toolkit. You don’t need to be a doctor to protect yourself. You just need to know what to ask, what to track, and what to watch for. Below, you’ll find exactly that.
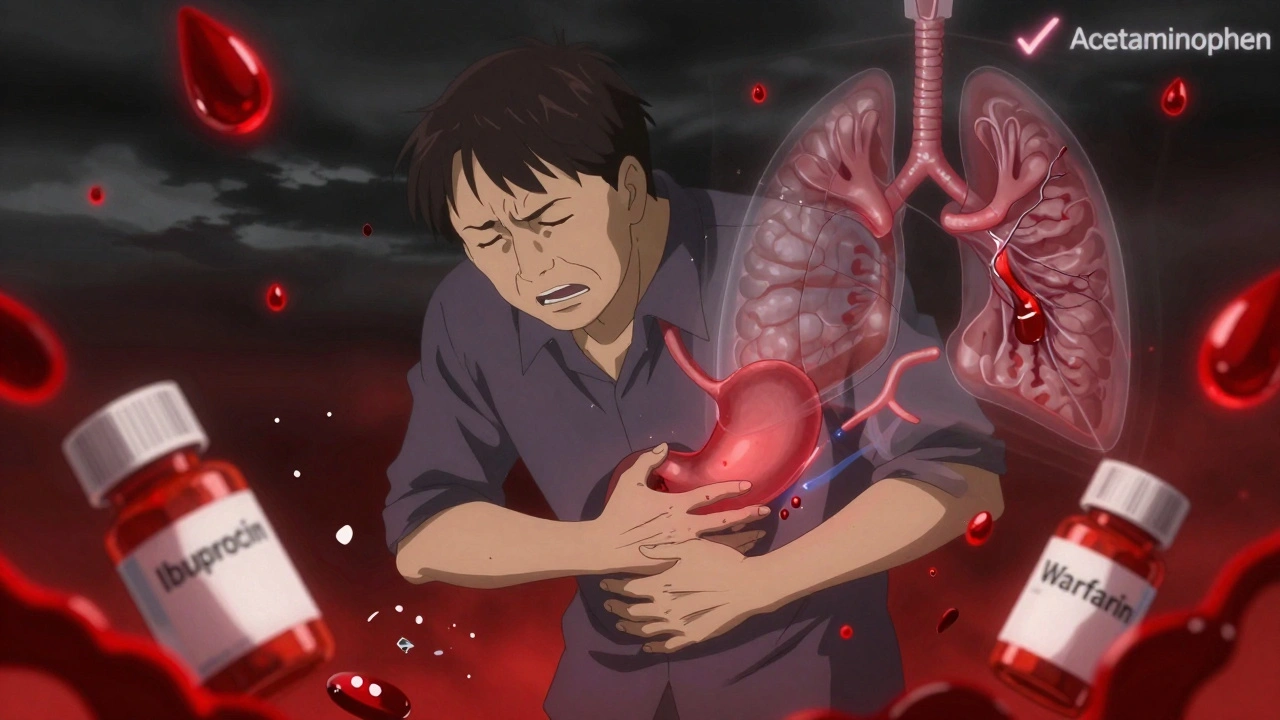
Blood Thinners and NSAIDs: Why This Drug Combo Can Be Life-Threatening
Combining blood thinners with NSAIDs like ibuprofen or naproxen can more than double your risk of dangerous bleeding. Learn why acetaminophen is the only safe OTC pain reliever and what alternatives actually work.