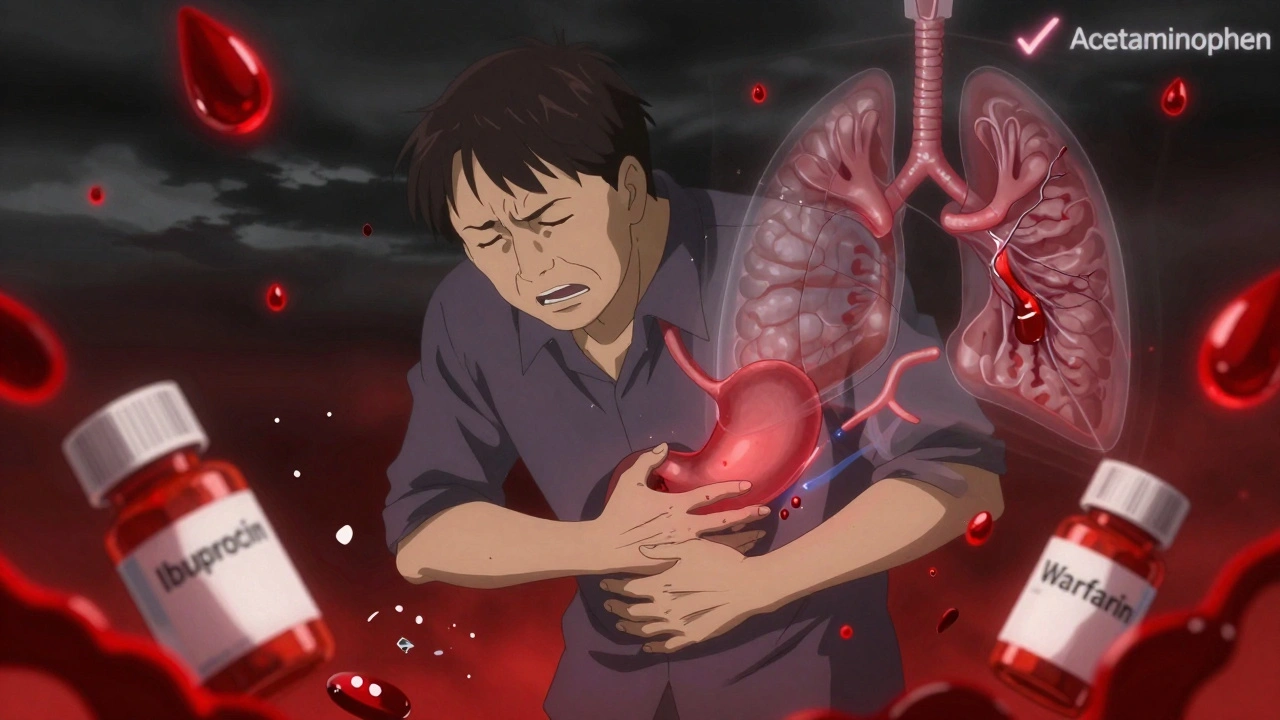
Combining blood thinners with common pain relievers like ibuprofen or naproxen isn’t just a bad idea-it’s a dangerous mix that can send you to the hospital, or worse. If you’re on a blood thinner for atrial fibrillation, a blood clot, or after a surgery, and you reach for an over-the-counter painkiller for your knee or back pain, you might be putting yourself at serious risk. This isn’t a myth. It’s not a "maybe." It’s a proven, measurable danger backed by data from over 50,000 patients.
What Happens When Blood Thinners and NSAIDs Mix?
Blood thinners-whether they’re warfarin, apixaban, rivaroxaban, or dabigatran-work by slowing down your blood’s ability to clot. That’s good if you’re trying to prevent a stroke or deep vein clot. But NSAIDs like ibuprofen, naproxen, and diclofenac don’t just reduce pain and inflammation. They also mess with your platelets, the tiny cells that help blood clot. They do this by blocking an enzyme called COX-1, which is needed to make substances that keep your stomach lining protected and your platelets sticky enough to seal cuts. When you take both, you’re hitting your body’s clotting system from two sides. Your blood thinners make it harder for clots to form. Your NSAIDs make it harder for your platelets to even try. The result? Bleeding that doesn’t stop easily. And it doesn’t just happen in your stomach.The Real Risk: It’s Not Just Stomach Bleeding
Most people think if you’re on blood thinners, the biggest danger is a stomach ulcer or black, tarry stools. But a massive 2024 study from Denmark, tracking 51,794 people on anticoagulants over 10 years, showed something more alarming: the bleeding risk spreads everywhere.- Gastrointestinal bleeding: 2.24 times more likely
- Intracranial bleeding (brain): 3.22 times more likely
- Pulmonary bleeding (lungs): 1.36 times more likely
- Urinary tract bleeding: 1.57 times more likely
Not All NSAIDs Are the Same
If you think all painkillers are equal when you’re on blood thinners, you’re wrong. The risk isn’t the same across the board.- Naproxen: Increases bleeding risk by 4.1 times
- Diclofenac: Increases bleeding risk by 3.3 times
- Ibuprofen: Increases bleeding risk by 1.79 times

Do Newer Blood Thinners Make It Safer?
You’ve probably heard that newer blood thinners like apixaban (Eliquis) or rivaroxaban (Xarelto) are better than warfarin. And they are-for preventing strokes and requiring fewer blood tests. But when it comes to mixing with NSAIDs? No difference. The Danish study confirmed it: whether you’re on warfarin or a DOAC, adding an NSAID still triples your risk of serious bleeding. So if you thought switching to a newer drug gave you a pass to take Advil, you’re mistaken. The danger is the same.Why Do People Keep Doing This?
It’s not because they’re careless. It’s because they don’t realize what they’re taking is a drug. Many people don’t think of ibuprofen or naproxen as "medications." They’re just "pain relievers." They grab them off the shelf like aspirin or vitamins. But they’re powerful drugs with serious side effects-especially when combined with anticoagulants. Doctors don’t always catch it either. A patient might say, "I only took one Advil," and the doctor assumes it’s harmless. But even that one pill can be enough to trigger bleeding in someone already on the edge.What Should You Take Instead?
The answer is simple: acetaminophen (Tylenol). Unlike NSAIDs, acetaminophen doesn’t affect platelets or the stomach lining. It doesn’t interfere with blood thinners. It’s the only over-the-counter pain reliever that’s consistently recommended for people on anticoagulants. If acetaminophen isn’t enough, here are other options:- Heat or ice packs for joint or muscle pain
- Physical therapy for chronic back or knee issues
- Topical pain creams with menthol or capsaicin
- Low-dose topical NSAIDs (like diclofenac gel)-these are absorbed through the skin, so they carry much less risk than pills

What About Stomach Protection? (PPIs Don’t Fix This)
Some doctors prescribe proton pump inhibitors (PPIs) like omeprazole to protect the stomach when someone takes NSAIDs. That helps reduce ulcers. But here’s the problem: PPIs don’t stop bleeding in the brain, lungs, or urinary tract. The Danish study made this clear: even with a PPI, the risk of intracranial or pulmonary bleeding stayed high. So if you think popping a stomach pill lets you safely take ibuprofen, you’re wrong. The danger isn’t just in your gut-it’s in your whole body.What Should You Do Right Now?
If you’re on a blood thinner:- Check your medicine cabinet. Do you have any NSAIDs? Naproxen? Ibuprofen? Diclofenac? Even if you haven’t taken them in months, keep them out of reach.
- Look at your pharmacy list. Have you been prescribed an NSAID recently? Ask your doctor if it’s still necessary.
- Next time you feel pain, reach for acetaminophen first. Not ibuprofen.
- Tell every doctor, pharmacist, and nurse you see that you’re on a blood thinner. Don’t assume they’ll check your list.
- If you’ve had unexplained bruising, dark stools, blood in urine, or sudden headaches, get checked immediately. These aren’t normal.
This Isn’t Just About One Pill
This isn’t a rare problem. In the U.S. alone, about 3 to 6 million people take blood thinners. And over 30 billion OTC ibuprofen tablets are sold every year. That’s a massive overlap. The American College of Cardiology says this combination is one of the most common-and preventable-drug interactions in older adults. It’s not just a medical error. It’s a public health blind spot. The fix? Awareness. Education. Better communication between patients and providers. And most of all-choosing acetaminophen over NSAIDs when you’re on blood thinners. Don’t wait for a bleeding episode to learn this lesson. The data is clear. The risks are real. And the safer alternative is right there on the shelf.Can I take Tylenol with blood thinners?
Yes, acetaminophen (Tylenol) is generally safe to take with blood thinners like warfarin, apixaban, or rivaroxaban. Unlike NSAIDs, it doesn’t affect platelets or increase bleeding risk. It’s the preferred over-the-counter pain reliever for people on anticoagulants. Still, always check with your doctor before starting any new medication, even if it’s available without a prescription.
Is ibuprofen ever safe with blood thinners?
No, ibuprofen is not considered safe with blood thinners. Even a single dose can increase your risk of bleeding by nearly 80%. Studies show it raises the chance of serious bleeding in the stomach, brain, lungs, and urinary tract. There’s no safe dose or duration. If you need pain relief, choose acetaminophen instead. If you’ve taken ibuprofen recently and are concerned, contact your doctor.
What’s the worst NSAID to take with blood thinners?
Naproxen carries the highest bleeding risk-4.1 times greater than taking a blood thinner alone. Diclofenac is next at 3.3 times higher risk. Both are strong COX-1 inhibitors, meaning they severely reduce platelet function and stomach protection. Even though they’re often prescribed for arthritis, they’re the most dangerous choices for people on anticoagulants. Avoid them completely if possible.
Do newer blood thinners like Eliquis or Xarelto have less risk with NSAIDs?
No. Whether you’re on warfarin, apixaban (Eliquis), rivaroxaban (Xarelto), or dabigatran (Pradaxa), combining any of them with NSAIDs increases your bleeding risk by the same amount. The type of blood thinner doesn’t change the danger. The problem isn’t the anticoagulant-it’s the NSAID. So don’t assume switching to a newer drug gives you permission to take Advil or Aleve.
Can a stomach pill like omeprazole protect me from NSAID bleeding?
No. Proton pump inhibitors (PPIs) like omeprazole can reduce the risk of stomach ulcers, but they don’t protect against bleeding in other parts of the body-like the brain, lungs, or kidneys. A major 2024 study showed that even with a PPI, the risk of intracranial and pulmonary bleeding stayed high when NSAIDs were taken with blood thinners. So don’t rely on stomach protection as a safety net. Avoid NSAIDs entirely if you’re on a blood thinner.
What should I do if I accidentally took ibuprofen with my blood thinner?
If you took one or two doses of ibuprofen or another NSAID by accident, don’t panic-but don’t ignore it either. Stop taking the NSAID immediately. Watch for signs of bleeding: unusual bruising, dark or bloody stools, vomiting blood, severe headaches, dizziness, or blood in urine. If you notice any of these, seek medical help right away. Even if you feel fine, mention the NSAID use at your next doctor’s visit. It’s better to be safe than to risk internal bleeding going unnoticed.
Are topical NSAIDs safer than pills for people on blood thinners?
Yes, topical NSAIDs like diclofenac gel are much safer than oral pills. Because they’re absorbed through the skin, very little enters your bloodstream. This means they’re less likely to interfere with blood thinners or cause internal bleeding. They can be a good option for localized pain like arthritis in the knee or elbow. But even then, avoid using them on large areas or for long periods without talking to your doctor.

Okay but what if the government is secretly pushing NSAIDs to make people bleed out so they can sell more blood thinners? I mean, look at the stats-30 BILLION ibuprofen tablets sold yearly? That’s not coincidence, that’s a plan. And who owns the pharmaceutical companies? WHO? The same people who control the WHO. Wake up. Acetaminophen? That’s just the next step in the opioid replacement agenda. They want you dependent on Tylenol so they can charge you $200 for a bottle of 500 pills. I’ve seen the documents. They’re in the basement of the FDA. I’ve got screenshots.
It’s fascinating-this isn’t just about pharmacology, it’s about how we perceive agency in our own bodies. We treat OTC drugs like candy because we’ve been conditioned to believe that ‘over-the-counter’ means ‘harmless.’ But the body doesn’t care about labels-it only responds to chemistry. And when you layer two systems that disrupt hemostasis, you’re not just increasing risk-you’re inviting chaos into a delicate equilibrium. The real tragedy? We’ve forgotten how to listen to our bodies. We numb, we mask, we ignore. And then we’re shocked when the system collapses. Maybe the solution isn’t just acetaminophen-it’s a cultural recalibration. Slow down. Feel the pain. Ask why it’s there.
Americans think they can medicate their way out of everything-then they wonder why they’re dying from ‘preventable’ causes. In India, we know pain. We don’t pop pills like candy. We rub oil, we rest, we endure. You people have a $200 billion pharmaceutical industry telling you that every ache needs a chemical fix. And now you’re surprised when your blood turns to water? Pathetic. Even your ‘safer’ acetaminophen? It’s liver poison if you take too much. But hey, at least it’s not an NSAID, right? You’re so proud of your ‘smart’ choices-when you’re just following ads from Big Pharma. Learn to sit with discomfort. It’s not a disease.
Thank you for writing this. I’ve been on apixaban for AFib for three years now, and I had no idea ibuprofen was such a risk-even one pill. I used to grab it for my tennis elbow without thinking. This is the kind of information that should be on every OTC bottle. I’m going to throw out my naproxen and keep Tylenol on hand now. Also, I’ll make sure my pharmacist knows about my meds every single time. Small steps, but this could literally save my life. Appreciate the clarity.
so like… ibuprofen is bad? but tylenol is good? weird how the whole medical world just… decided that? like what if tylenol is just the new thing they want us to take so they can charge more? also i heard it causes liver damage? so… what do we even do??
You’re not alone in feeling overwhelmed by this. I was terrified when I first found out I was on a blood thinner-and then realized I’d been taking Advil for years. But you’re doing great just by reading and asking questions. Start small: swap one pill at a time. Replace your ibuprofen with Tylenol this week. Try a heating pad for your back. Talk to your doctor about topical gels-they’re a game changer. You don’t have to fix everything overnight. Just keep choosing the safer option, one day at a time. You’ve got this.
Oh wow. So after 50,000 patients, we finally figured out that mixing poison with poison = more poison? Congrats, science. I’ve been telling people this since 2018. Meanwhile, your doctor probably still gives you a prescription for naproxen like it’s a gift. The real question is: why are you still trusting people who don’t know the difference between a COX-1 and a COX-2? You think your pharmacist is reading your file? Nah. They’re scanning barcodes. You’re a number. Wake up.
I love how this post reads like a love letter to the liver-poetic, precise, and devastatingly tender. The way you describe NSAIDs as saboteurs in the symphony of hemostasis? Chilling. And the fact that PPIs are the placebo priests of the GI tract, chanting mantras of safety while the brain bleeds in silence? That’s literature. I’ve been using diclofenac gel for my arthritic knuckles-yes, it’s a whisper of the drug, not a shout-and I feel like a rebel. Not because I’m defying doctors, but because I’m listening to my body’s quiet, trembling voice. And yes-I threw out my ibuprofen. I replaced it with chamomile tea, a warm compress, and the courage to sit with discomfort. Pain isn’t always the enemy. Sometimes, it’s the messenger. And we’ve been shooting the messengers for decades.