Blood Thinners: What They Are, How They Work, and What You Need to Know
When your blood clots too easily, it can lead to strokes, heart attacks, or deadly blockages in your legs or lungs. That’s where blood thinners, medications that reduce your blood’s ability to form clots. Also known as anticoagulants or antiplatelets, they don’t actually make your blood thinner—they just slow down the clotting process to keep things flowing safely. If you’ve been prescribed one, you’re not alone. Millions use them after heart surgery, for atrial fibrillation, or after a deep vein thrombosis. But they’re not simple pills. Taking them wrong can be just as dangerous as not taking them at all.
There are two main types: anticoagulants, like warfarin and rivaroxaban, which target clotting factors in your blood, and antiplatelets, like aspirin and clopidogrel, which stop platelets from sticking together. Each has different rules. Warfarin needs regular blood tests and fights with vitamin K in foods like spinach and broccoli. Newer ones like apixaban don’t need testing but still clash with some antibiotics, antifungals, and even St. John’s wort. And yes—some of these interactions show up in your medicine cabinet even if you didn’t think they mattered. That’s why managing multiple meds safely, as covered in our posts, isn’t optional. It’s life-saving.
Blood thinners don’t just affect your body—they affect your daily life. You might need to rethink your diet, your exercise routine, or even how you brush your teeth. A cut that used to stop bleeding in seconds now might ooze longer. A fall could mean internal bleeding you don’t feel until it’s serious. That’s why knowing when to call your doctor about swelling, bruising, or strange headaches matters more than ever. And if you’re traveling abroad, carrying these meds safely becomes a whole other challenge—especially when you’re in a country with different rules or no access to your usual pharmacy. You also can’t just stop them on your own. Tapering off needs planning, just like with steroids or antidepressants. Skipping a dose or quitting cold turkey can trigger a clot when your body isn’t ready.
What you’ll find in the posts below isn’t just theory. It’s real advice from people who’ve been there: how to avoid dangerous drug interactions, what to do if you miss a dose, how to store your pills safely at home, and why some people feel worse after switching to generics—even when the chemistry says it’s the same. You’ll also see how insurance and pharmacy pricing can make your copay higher than the cash price, and why knowing your options matters. These aren’t hypotheticals. They’re daily realities for anyone on blood thinners.
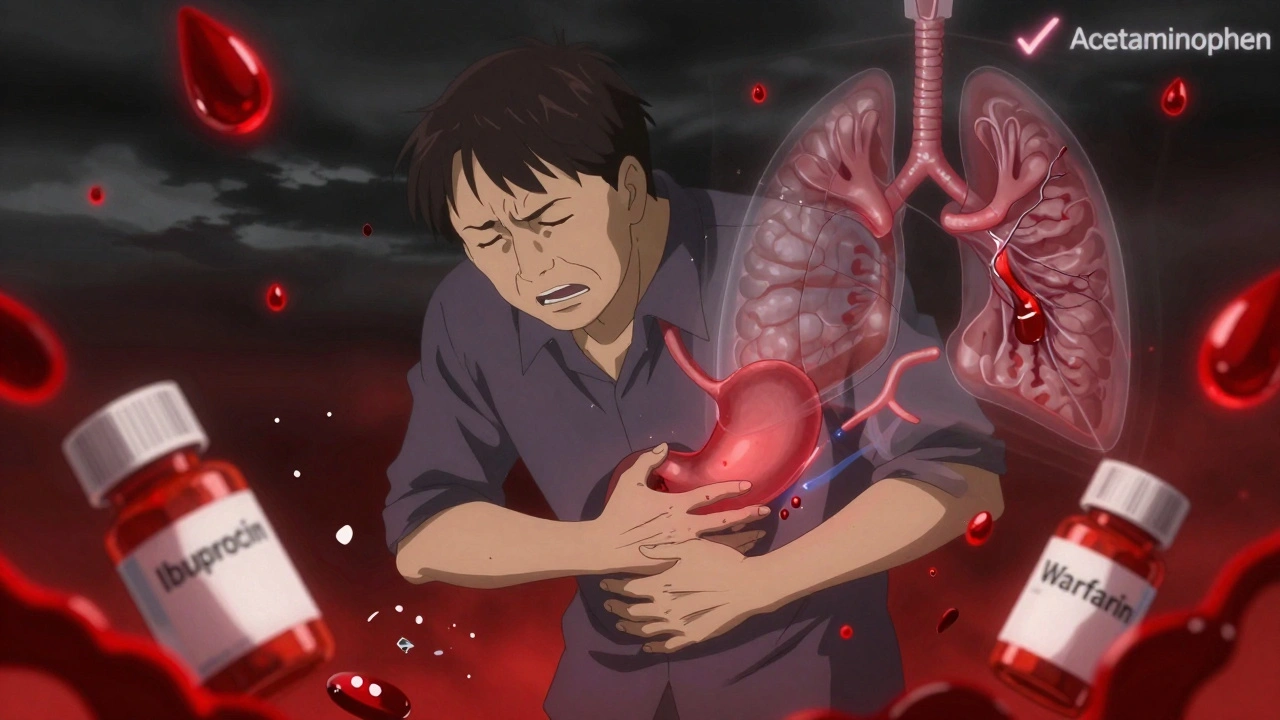
Blood Thinners and NSAIDs: Why This Drug Combo Can Be Life-Threatening
Combining blood thinners with NSAIDs like ibuprofen or naproxen can more than double your risk of dangerous bleeding. Learn why acetaminophen is the only safe OTC pain reliever and what alternatives actually work.