Statin Diabetes Risk Calculator
Assess Your Risk
This calculator helps you understand how your personal health profile affects your risk of developing diabetes while taking statins. It's based on research from the article above.
Many people take statins to lower their cholesterol and protect their heart. But if you’ve noticed your blood sugar creeping up after starting one, you’re not alone. Research shows that statins can raise blood sugar levels in some people - enough to push a few over the line into type 2 diabetes. It’s not common, but it’s real. And knowing how it works can help you make smarter choices.
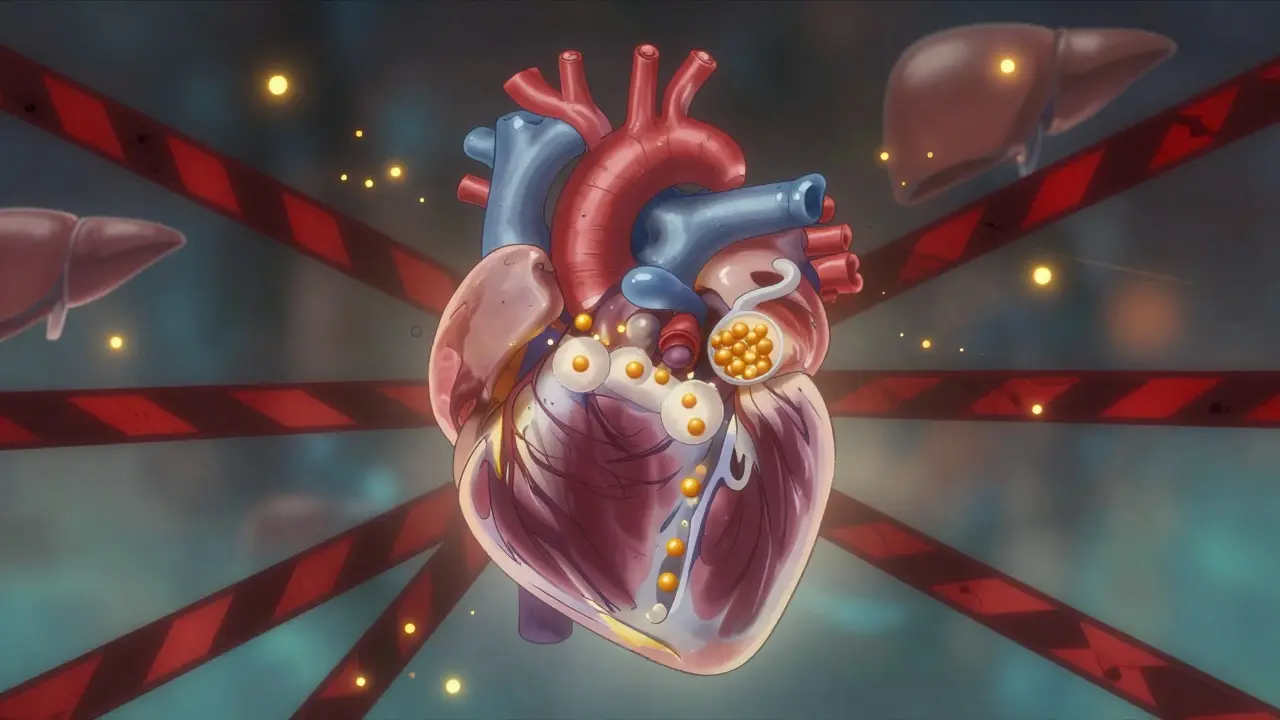
How Statins Affect Blood Sugar
Statins work by blocking a liver enzyme called HMG-CoA reductase. That stops your body from making too much cholesterol. But that same blockage also messes with other molecules your body needs - like CoQ10 and isoprenoids - which play a role in how insulin works. Without them, your muscles and fat cells don’t respond as well to insulin. That’s called insulin resistance. Your pancreas then tries to compensate by pumping out more insulin. Over time, the beta cells in your pancreas get worn out. They can’t keep up. Blood sugar rises.
This isn’t just theory. A 2023 analysis of nearly 9,000 people in Finland found that those on statins had a 46% higher chance of developing type 2 diabetes over six years. Insulin sensitivity dropped by 24%. Insulin production fell by 12%. Another study showed that just 10 weeks of high-dose atorvastatin increased insulin resistance significantly. The body tried to make up for it by releasing more insulin - but not enough to keep glucose in check.
Who’s Most at Risk?
Not everyone on statins develops higher blood sugar. The risk is highest for people who already have metabolic trouble. If you have prediabetes, belly fat, high triglycerides, low HDL, or high blood pressure, you’re more likely to see your glucose levels climb. Genetics matter too. Some people carry a variant in the SLCO1B1 gene that makes them more sensitive to statin-induced glucose changes.
Age plays a role. People over 65 are more vulnerable. Women with polycystic ovary syndrome (PCOS) or a history of gestational diabetes are also at higher risk. And it’s dose-dependent. High-intensity statins - like 40-80 mg of atorvastatin or 20-40 mg of rosuvastatin - carry a 36% higher risk of new diabetes compared to placebo. Lower doses? Around 10% higher risk.
Other meds can make it worse. If you’re taking steroids, beta-blockers, or certain diuretics, your risk goes up. So does being sedentary or eating a lot of refined carbs. Lifestyle doesn’t cause the statin effect - but it can turn a small glucose bump into full-blown diabetes.
How Big Is the Risk?
Let’s put numbers to it. For every 100 people taking a statin for five years, about 1 to 2 will develop type 2 diabetes because of it. That’s 0.1% to 0.3% per year. Sounds small? It is. But here’s the flip side: in that same group, 1.5 to 2 people will avoid a heart attack or stroke. The benefit wins - by a lot.
For someone with existing heart disease, the numbers are even more one-sided. Statins reduce their risk of another heart attack by up to 30%. The diabetes risk? Less than 1 in 100. That’s why doctors don’t stop prescribing statins to people with a history of heart problems. The risk of dying from a heart attack is far greater than the risk of needing diabetes meds.
But for someone with no heart disease - just high cholesterol - the balance is tighter. If you’re young, lean, and active with borderline cholesterol, the diabetes risk might tip the scales. That’s why doctors now screen for prediabetes before starting statins.

Which Statins Are Riskiest?
Not all statins are the same when it comes to blood sugar. Atorvastatin and rosuvastatin - the high-intensity ones - have the strongest link to increased glucose. Simvastatin and pravastatin carry lower risk. Pitavastatin might even be neutral or slightly protective in some studies.
Here’s a quick breakdown:
| Statin | Typical Dose | Intensity | Diabetes Risk Compared to Placebo |
|---|---|---|---|
| Atorvastatin | 40-80 mg | High | +36% |
| Rosuvastatin | 20-40 mg | High | +36% |
| Simvastatin | 40 mg | Medium | +18% |
| Pravastatin | 40 mg | Medium | +10% |
| Pitavastatin | 2-4 mg | Medium | +5% or neutral |
That doesn’t mean you should switch statins on your own. But if you’re newly diagnosed with prediabetes and need a statin, asking your doctor about pravastatin or pitavastatin could make sense.
What Should You Do If You’re on Statins?
If you’re already taking a statin, don’t stop. The consequences of stopping - heart attack, stroke, death - are far worse than the risk of diabetes.
Instead, do this:
- Get your blood sugar checked before starting, and again 3-6 months after. Fasting glucose and HbA1c are the best markers.
- If your HbA1c rises above 5.7%, talk to your doctor. You might have prediabetes. That doesn’t mean you need meds - lifestyle changes can reverse it.
- Move more. Just 150 minutes a week of brisk walking cuts diabetes risk by 58% in people on statins.
- Eat fewer refined carbs. White bread, sugary drinks, and pastries spike glucose. Swap them for whole grains, beans, vegetables, and healthy fats.
- Watch your weight. Losing 5-10% of body weight can restore insulin sensitivity - even if you’re on statins.
Some people report needing to start metformin or adjust their diabetes meds after beginning statins. That’s normal. It’s not a failure - it’s your body adapting. Your doctor can help you fine-tune things.
Can You Reverse the Effect?
Yes - in some cases. When people stop statins, their insulin sensitivity often improves within weeks. Blood sugar levels drop back down. But here’s the catch: if you’ve already developed type 2 diabetes, stopping the statin won’t cure it. And if you had heart disease, stopping could put you at serious risk.
So reversal only makes sense if you were on statins for primary prevention - meaning you had no heart disease, just high cholesterol - and you developed prediabetes. In that case, your doctor might lower the dose, switch statins, or pause treatment temporarily while you focus on lifestyle changes.
What Experts Say
The American Heart Association, the American Diabetes Association, and the European Atherosclerosis Society all agree: don’t avoid statins because of diabetes risk. The benefits for heart health are too strong.
Dr. Steven Nissen from Cleveland Clinic puts it plainly: "The risk of diabetes from statins is real, but it’s small. The risk of a heart attack without them is enormous. We don’t stop using seatbelts because they can cause minor bruising."
The CDC says the same: "Statins can stop your body’s insulin from working well. But for most people, the heart protection they offer is worth it."
The key is awareness. If you’re at risk, monitor. If you’re not, don’t panic. Statins aren’t causing a diabetes epidemic. They’re helping millions live longer.
The Bottom Line
Statins can raise blood sugar - but only in a small group of people who are already on the edge. For most, the heart benefits far outweigh the risk. If you’re on a statin, get your glucose checked. If you’re prediabetic, focus on food, movement, and weight. Don’t quit the statin. Talk to your doctor about options. And remember: managing cholesterol isn’t about avoiding side effects. It’s about living longer - and healthier - with fewer heart problems down the road.
Do statins cause diabetes?
Statins don’t directly cause diabetes, but they can raise blood sugar enough to push some people over the diagnostic threshold - especially those with prediabetes, obesity, or metabolic syndrome. The increase is small and affects only a minority of users.
Which statin has the least diabetes risk?
Pravastatin and pitavastatin appear to have the lowest risk of raising blood sugar. Atorvastatin and rosuvastatin carry the highest risk, especially at high doses. But the choice depends on your cholesterol levels and heart risk - not just diabetes risk.
Should I stop taking statins if my blood sugar goes up?
No - unless your doctor advises it. Stopping statins increases your risk of heart attack and stroke far more than the risk of developing diabetes. Instead, work with your doctor to adjust your treatment plan - maybe lower the dose, switch statins, or add lifestyle changes.
Can lifestyle changes reduce the diabetes risk from statins?
Yes. Regular exercise, losing excess weight, cutting refined carbs, and eating more fiber can improve insulin sensitivity and offset the glucose-raising effect of statins. In fact, lifestyle changes are often more effective than adding diabetes medication.
How often should I check my blood sugar if I’m on statins?
Get a fasting glucose and HbA1c test before starting statins. Then repeat the tests 3 to 6 months after beginning treatment. If you’re at high risk for diabetes (prediabetes, obesity, family history), your doctor may recommend checking every 6 to 12 months.

Statins gave me prediabetes. Stopped them. Blood sugar back to normal in 2 months. Doctors don't get it. Your heart doesn't matter if you're diabetic.
i just started taking pravastatin last month and my fasting glucose went from 98 to 107. i didnt think it was related until i read this. im gonna ask my doc about switching. also i started walking 30 mins a day and my numbers are already dropping. maybe its not all bad?
Let’s be brutally honest: this is pharmaceutical capitalism in its purest form. You’re told to take a drug that subtly sabotages your metabolic health so you can live 2.3 years longer-while the company makes billions. The ‘benefit-risk’ calculus is a myth engineered by lipidologists with conflict-of-interest disclosures buried in footnotes. The real question isn’t whether statins raise glucose-it’s why we’re still treating cholesterol like a villain instead of addressing systemic inflammation, insulin resistance, and ultra-processed food environments. This isn’t medicine. It’s pharmacological appeasement.
Interesting how the article cherry-picks the 2023 Finnish study while ignoring the 2021 meta-analysis in The Lancet showing no significant increase in diabetes incidence with low-to-moderate intensity statins in non-prediabetic populations. Also, the ‘1 in 100’ diabetes risk is misleading-it’s not a linear function of dose, it’s a threshold effect in genetically susceptible individuals. Most people on statins never develop diabetes. But you’ll never hear that from the fear-mongering blogs. The real epidemic here is medical overinterpretation.
So let me get this straight-take a pill that might turn you diabetic so you don’t die of a heart attack you caused by eating 12 donuts a week? Brilliant. I’m sure the cardiologist’s yacht is paid off. Meanwhile, the only thing statins are good for is giving people permission to keep eating like garbage. ‘Oh I’m on a statin, I’m covered.’ No you’re not. You’re just a walking glucose spike with a prescription.
I’ve been on atorvastatin for 8 years. My HbA1c went from 5.4 to 6.1. I was terrified. I stopped reading the news, started doing yoga, cut out all white carbs, and added 10k steps a day. My A1c is now 5.5 again. I didn’t stop the statin. I didn’t need metformin. I just stopped being a lazy sack. The body isn’t broken-it’s just being ignored. Statins aren’t the enemy. Your lifestyle is. And if you’re blaming the pill instead of your breakfast cereal, you’re not sick-you’re in denial. I’ve seen people go from prediabetes to normal without meds. It’s not magic. It’s discipline. And yes, I still take my statin. Because I don’t want to be dead at 60 while my kids wonder why I didn’t just walk more.
It is imperative to recognize that the statistical probability of cardiovascular event reduction far exceeds the marginal risk of statin-induced glucose dysregulation. The physiological mechanisms are well-documented and the clinical guidelines are unequivocal. To discontinue therapy based on anecdotal glucose fluctuations is to endanger life. Prioritize evidence over emotion. Your health is not a referendum. It is a responsibility.
They say the risk is small. But what if you’re the one? What if your pancreas gives up because of a pill you were told was ‘safe’? You think your doctor cares when your A1c hits 6.5? They’ll just add another pill. And another. And another. And you’ll be on metformin, GLP-1s, insulin-while they keep prescribing the statin because ‘the heart comes first.’ But what if your heart’s fine and your liver’s screaming? Who’s listening? No one. They’re all too busy counting the dollars. I’m not stopping my statin. But I’m never trusting another ‘benefit-risk’ chart again.