Diabetes Medication Decision Guide
Recommended Medication
Why this recommendation?
Cost considerations
When you or someone you know is living with type 2 diabetes, picking the right oral medication can feel like navigating a maze. Precose is the brand name for Acarbose, an alpha‑glucosidase inhibitor that slows carbohydrate absorption in the gut. But it’s not the only option on the shelf. This guide walks you through how Acarbose stacks up against the most common alternatives, so you can see which drug aligns with your health goals, lifestyle, and budget.
How Acarbose Works - The Basics
Acarbose inhibits the enzyme alpha‑glucosidase in the small intestine, delaying the breakdown of complex carbs into glucose. The result is a smoother rise in blood sugar after meals, which helps keep HbA1c levels in check without triggering a dramatic insulin surge.
Key attributes of Acarbose:
- Typical dose: 50 mg three times daily with the first bite of each main meal.
- Onset: Works within 30 minutes of eating.
- Side‑effect profile: Mostly gastrointestinal - gas, bloating, and mild diarrhea.
Top Alternatives to Acarbose
Below are the most frequently prescribed oral agents that target blood‑sugar control through different pathways. Each has its own strengths and trade‑offs.
Miglitol is another alpha‑glucosidase inhibitor, chemically similar to Acarbose but with a slightly shorter half‑life. It’s taken at 25 mg with meals and tends to cause less flatulence, though nausea can still appear.
Voglibose is popular in Asian markets, offering a once‑daily dose option for patients who struggle with three‑times‑daily regimens. Its efficacy mirrors Acarbose, but it’s less widely available in Australia.
Metformin belongs to the biguanide class and works by reducing hepatic glucose production and improving insulin sensitivity. It’s often the first‑line drug because it’s cheap, weight‑neutral, and has an extensive safety record.
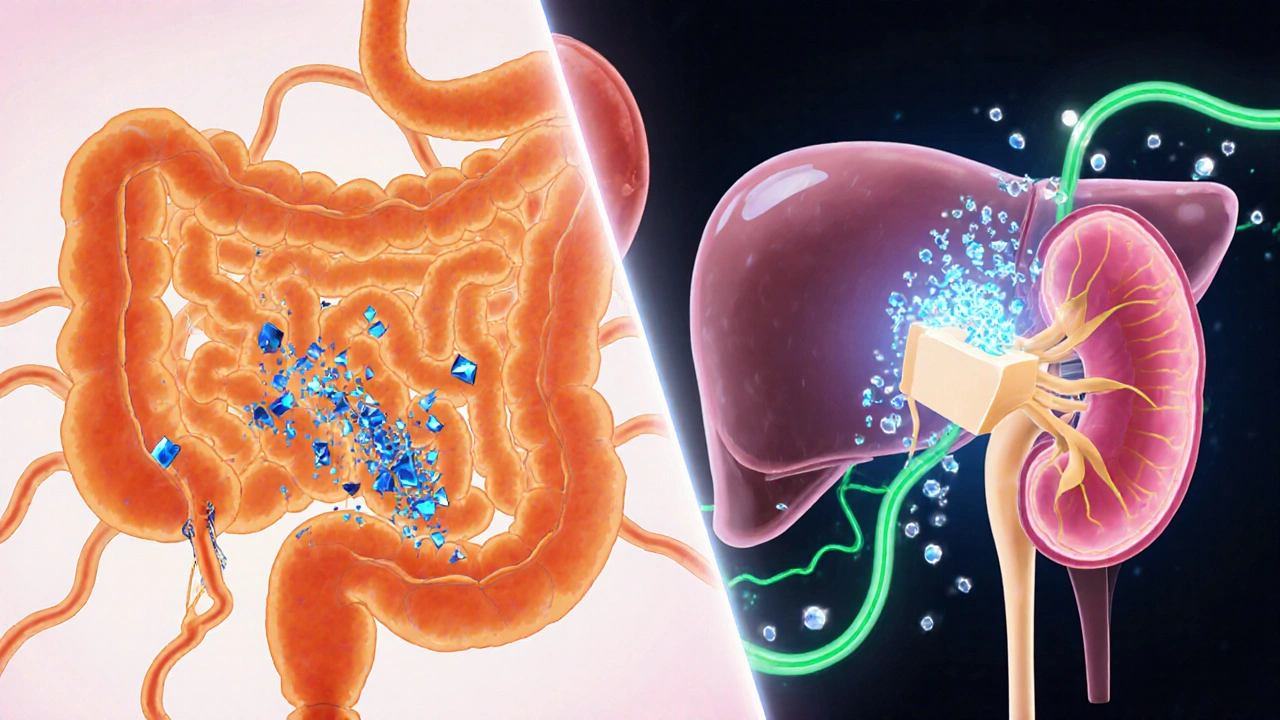
SGLT2 inhibitors such as dapagliflozin and empagliflozin lower blood sugar by blocking glucose reabsorption in the kidneys, causing it to be expelled in urine. They also bring cardiovascular and renal benefits but can raise the risk of urinary tract infections.
GLP‑1 receptor agonists like liraglutide act on the gut‑brain axis to increase insulin secretion, suppress appetite, and slow gastric emptying. Though injectable, they excel at weight loss and heart‑health protection.
Side‑Effect Showdown
Side effects often decide whether a patient sticks with a medication. Here’s a quick glance at the most common complaints for each drug class.
| Drug | Typical Side Effects | Serious Risks |
|---|---|---|
| Acarbose | Flatulence, abdominal pain, mild diarrhea | Rare hypoglycemia when combined with insulin or sulfonylureas |
| Miglitol | Nausea, occasional bloating | Hypoglycemia with concurrent insulin |
| Voglibose | Gas, soft stools | Very low, but monitor for hypoglycemia |
| Metformin | Gastro‑intestinal upset, metallic taste | Lactic acidosis (extremely rare, usually with renal impairment) |
| SGLT2 inhibitors | Increased urination, mild genital itching | UTI, ketoacidosis, rare amputations |
| GLP‑1 agonists | Nausea, vomiting, constipation | Pancreatitis (rare), gallbladder disease |
Cost Considerations in Australia (2025)
Price can be a deal‑breaker, especially when medications aren’t fully covered by the PBS. Below is an approximate monthly out‑of‑pocket cost for a typical dose, based on 2025 Australian pharmacy pricing.
| Drug | PBS Status | Monthly Cost |
|---|---|---|
| Acarbose (Precose) | Not listed | ~120 |
| Miglitol | Not listed | ~115 |
| Voglibose | Limited PBS use | ~130 |
| Metformin | PBS‑listed | ~15 |
| SGLT2 inhibitors (e.g., dapagliflozin) | PBS‑listed for high‑risk patients | ~45-70 |
| GLP‑1 agonists (e.g., liraglutide) | PBS‑listed for obesity/diabetes with complications | ~180 |
When Acarbose Makes Sense
If you’re already on a regimen that includes metformin or a sulfonylurea but still see post‑meal spikes, Acarbose can be the missing piece. It works without causing weight gain, which is a plus for patients already struggling with obesity.
Because its primary action is at the intestinal level, Acarbose is also safe for people with mild renal impairment-something you need to double‑check with a doctor before starting SGLT2 inhibitors.
Key scenarios where Acarbose shines:
- Predominant carbohydrate‑rich diet (e.g., Asian cuisines with rice and noodles).
- Need for a non‑systemic drug that doesn’t affect liver or kidney function.
- Patients who have contraindications to metformin (e.g., severe GI intolerance).
When Alternatives Might Be Better
If you’re looking for weight loss, cardiovascular protection, or a once‑daily pill, the newer classes often win.
Metformin remains the workhorse for most newly diagnosed patients because of its proven track record and low price.
SGLT2 inhibitors add heart‑failure and kidney‑disease benefits, making them a go‑to for patients with those comorbidities.
GLP‑1 agonists are the top pick for patients who need significant weight reduction-clinical trials show up to 15% body‑weight loss in a year.
In practice, doctors frequently stack Acarbose with metformin to tame post‑prandial peaks while still harvesting metformin’s fasting‑glucose control.
Practical Tips for Starting Acarbose
- Begin with a low dose (25 mg) at the first bite of your largest meal.
- Gradually increase every 1-2 weeks to the target 50 mg three times daily, watching for GI discomfort.
- Take it with food-if you miss a meal, skip the dose rather than taking it on an empty stomach.
- Stay hydrated; increased water intake helps mitigate constipation.
- Inform your pharmacist that you’re on Acarbose before purchasing over‑the‑counter supplements, especially ones containing fiber or sorbitol, as they can amplify the gas‑producing effect.
Quick Decision Checklist
- Do you have frequent post‑meal glucose spikes? → Acarbose or miglitol.
- Is cost a primary concern? → Metformin or generic SGLT2 (if PBS‑eligible).
- Seeking weight loss? → GLP‑1 agonist.
- Kidney issues? → Acarbose (monitor for hypoglycemia with insulin).
- Prefer once‑daily dosing? → Voglibose or SGLT2 inhibitors.
Frequently Asked Questions
Can I take Acarbose with insulin?
Yes, but you’ll need to adjust your insulin dose. Acarbose flattens post‑meal spikes, so a lower bolus may be enough. Always coordinate changes with your endocrinologist.
How quickly does Acarbose start working?
It begins to inhibit carbohydrate absorption within about 30 minutes after the first bite, making it ideal for meals you plan ahead of time.
Is Acarbose safe for people over 70?
Generally, yes, as long as kidney function is monitored. The drug’s action stays in the gut, so systemic exposure is low. Discuss dosage with your doctor.
Why does Acarbose cause gas?
Undigested carbohydrates reach the colon, where bacteria ferment them, producing hydrogen and methane-hence the flatulence. Starting at a low dose and gradually increasing can reduce this effect.
Can I switch from Acarbose to a SGLT2 inhibitor?
You can, but a wash‑out period isn’t required. Your doctor will likely taper Acarbose while starting the SGLT2 inhibitor to avoid overlapping GI side effects and to monitor glucose trends.
Choosing a diabetes medication isn’t a one‑size‑fits‑all decision. By weighing mechanism, side‑effects, cost, and personal health goals, you can find a regimen that keeps your blood sugar steady and your life moving forward.



Hey folks, if you’re just getting started with Acarbose, the key is to go slow – a 25 mg tablet with your biggest meal, then titrate up every week or two.
Give your gut a chance to adapt and keep a water bottle handy; staying hydrated really helps ease the occasional bloating.
Don’t forget to pair it with a balanced plate – protein and healthy fats can smooth out any lingering spikes.
And if the gas gets out of hand, dialing back the dose for a few days is totally fine before you push it up again.
Acarbose acts as a competitive inhibitor of the brush‑border α‑glucosidases, specifically targeting sucrase, maltase and isomaltase.
By binding to the active site, it delays polysaccharide hydrolysis, allowing a larger fraction of carbohydrate to reach the colon where bacterial fermentation occurs.
This results in a flatter post‑prandial glucose excursion without markedly affecting fasting glucose.
Because the effect is confined to the intestinal lumen, systemic exposure is minimal, which explains the low incidence of hypoglycemia unless combined with insulin or sulfonylureas.
Let me be perfectly clear: the pharmaceutical industry has turned diabetes treatment into a marketing battleground, and the average patient is left to navigate a maze of glossy brochures and half‑truths.
They push newer, brand‑name SGLT2 inhibitors and GLP‑1 agonists with promises of heart‑health miracles while hiding the fact that many of these drugs carry serious risks like ketoacidosis and rare amputations.
Meanwhile, a decades‑old generic like Metformin sits on the shelf, cheap, well‑studied, and backed by a mountain of outcome data, yet it’s dismissed by “innovators” as “old‑fashioned.”
Then there’s Acarbose – an enzyme inhibitor that essentially tells your gut to slow down, a humble approach that respects the body’s natural digestion rather than hijacking hormonal pathways.
Sure, the side‑effects include gas and occasional diarrhea, but those are far less frightening than the prospect of a urinary tract infection that could land you in the hospital.
The moral failing here is the neglect of cost‑effectiveness; patients in Australia are paying over a hundred dollars a month for a drug that isn’t even PBS‑listed, while Metformin is a fraction of that price.
When you weigh the evidence, the decision isn’t about flashier pills; it’s about sustainable, evidence‑based care that doesn’t bankrupt the patient.
Healthcare providers have an ethical duty to present the full spectrum of options, not just the ones with the biggest profit margins.
We must stop glorifying novelty for its own sake and start championing what truly works in the long run.
If you’re a clinician, ask yourself whether you’re recommending a drug because it’s the best fit for the patient’s physiology and wallet, or because it’s the latest product you were trained to sell.
Patient autonomy is meaningless if the choices presented are skewed by corporate incentives.
In the end, Acarbose may not be the flashiest option, but it embodies a principle of modesty and practicality that should be celebrated, not sidelined.
So, let’s bring the conversation back to outcomes, affordability, and the real lived experience of managing a chronic disease, instead of getting lost in a haze of hype.
Ultimately, the choice should be patient‑centric, driven by data, not by a brand’s marketing budget.
A balanced approach that integrates cost, efficacy, and quality of life will always outshine hype.
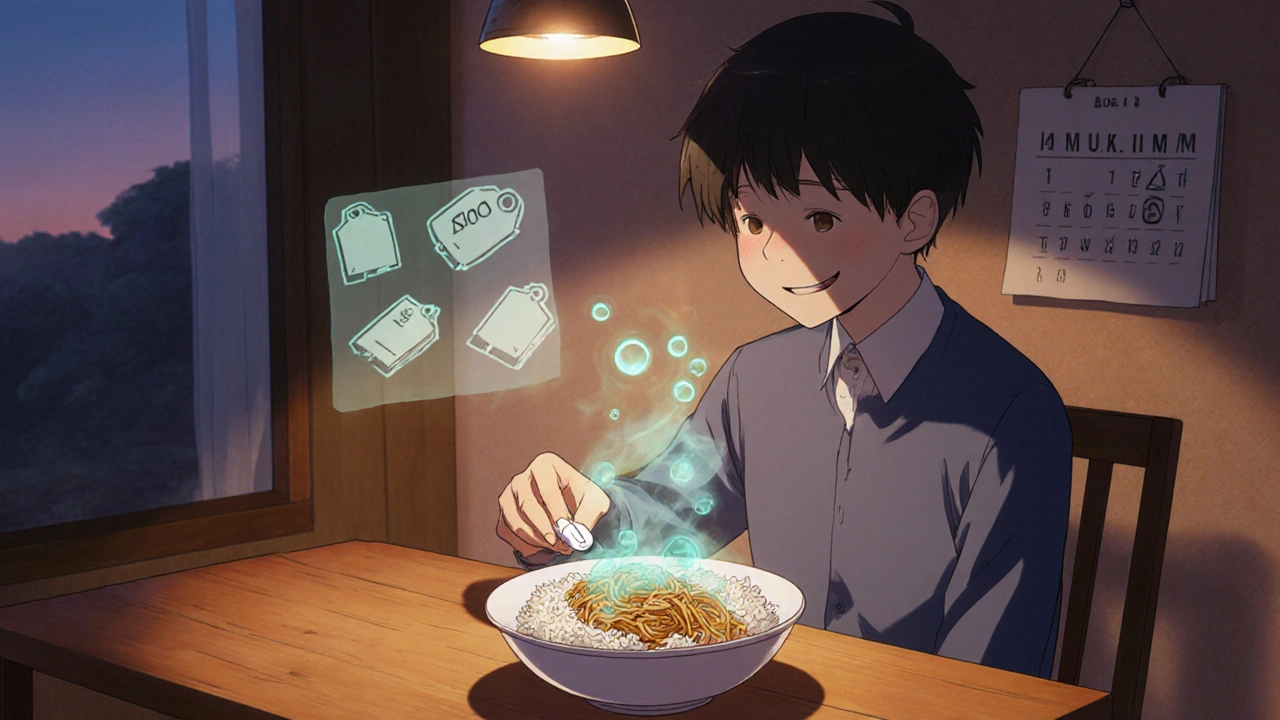
While the debate about cost and novelty is certainly valid, it’s worth remembering that cultural dietary patterns heavily influence drug choice.
In communities where staple meals are high in complex carbohydrates, an α‑glucosidase inhibitor like Acarbose can align neatly with traditional eating habits, reducing post‑meal spikes without altering the flavor profile of familiar dishes.
Watch the gut gas when you dial up Acarbose.
The price tag on Acarbose feels like a tragedy in a market that glorifies profit over patients.
I get that the gastrointestinal side‑effects can be a real hurdle, especially if you’ve got a busy life.
Try starting with a half dose and slowly building up; many folks find the gas subsides after a couple of weeks.
If it still feels too much, talk to your doctor about switching or combining with a low‑dose Metformin to balance things out.
Acarbose fits well for people who eat rice heavy meals it slows carb absorption and keeps glucose steady
That claim overlooks the fact that relying on an enzyme inhibitor alone can leave patients vulnerable to unexpected spikes when meal composition varies wildly.
It’s understandable to feel uneasy about the flatulence – it’s a common reaction, but remember that the gut microbiome adapts over time.
If the discomfort persists, a gentle taper and probiotic support can make the transition smoother, and your healthcare team is there to help fine‑tune the regimen.
One must appreciate that the pharmacodynamic nuance of α‑glucosidase inhibition is a testament to sophisticated therapeutic design, a subtlety often eclipsed by the fanfare surrounding cardioprotective SGLT2 agents; nevertheless, the latter’s market dominance speaks more to commercial choreography than to pure scientific merit.