Corticosteroid Tapering Calculator
Stopping corticosteroids like prednisone or prednisolone isn’t as simple as taking your last pill and calling it done. If you’ve been on these meds for more than a few weeks, your body has adjusted. Your adrenal glands have slowed down cortisol production because the drug was doing the job for them. Suddenly removing it? That’s when things go sideways. Fatigue hits like a brick. Muscles ache. Mood swings creep in. And if you’re not prepared, you could end up in the ER thinking it’s a flare-up-when it’s actually your body begging for time to recover.
Why Tapering Isn’t Optional
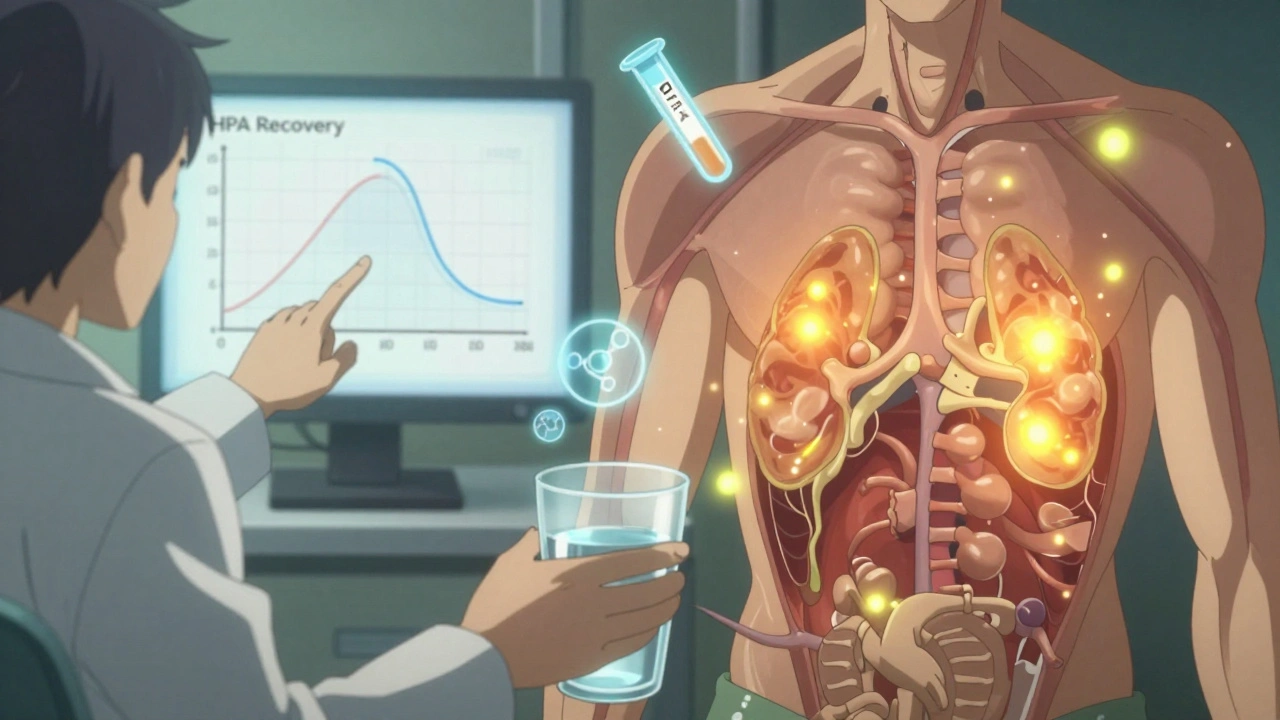
Doctors don’t recommend tapering just to be cautious. It’s medical necessity. When you take corticosteroids daily for more than two to four weeks-especially at doses over 7.5 mg of prednisolone-you suppress your own HPA axis. That’s the hypothalamic-pituitary-adrenal system, the body’s natural cortisol factory. Without a slow, controlled reduction, your adrenals can’t snap back fast enough. The result? Withdrawal symptoms show up in 78% of people who quit cold turkey, according to clinical data from the Journal of Clinical Endocrinology & Metabolism.
These aren’t minor inconveniences. People report crushing fatigue, joint pain so bad they can’t get out of bed, nausea, trouble sleeping, and even depression. And here’s the twist: many mistake these symptoms for a disease flare. A rheumatoid arthritis patient might think their joints are swelling again. Someone with Crohn’s might assume their gut is acting up. But if you’re not seeing new inflammation markers, it’s likely withdrawal-not disease activity.
How Fast Should You Taper?
There’s no one-size-fits-all schedule. The pace depends on how long you’ve been on steroids and your starting dose. For someone on high-dose therapy-say, 40 mg of prednisone daily-the first step is often a quick drop. You might reduce by 5 mg every 3 to 7 days until you hit around 15 mg. That’s the point where things slow down.
Once you’re below 15 mg, the rule changes. Now you drop by 1 mg every 1 to 2 weeks. Why? Because this is where your body starts to wake up. This is the phase where most withdrawal symptoms pop up. The Australian Prescriber found that 63% of patients report symptoms when doses fall below 15 mg daily. That’s why rushing here is risky.
For those who’ve been on steroids for months or years, the taper can stretch out for six months or longer. One patient in a Case Reports in Rheumatology study completed a 26-week taper from 40 mg to zero-without a single symptom. How? They followed a strict, slow, structured plan backed by their rheumatologist and endocrinologist.
What Symptoms Should You Watch For?
Not all bad feelings mean you’re in trouble. But knowing the difference saves you from unnecessary panic-or worse, a dangerous dose increase.
- Withdrawal syndrome: General tiredness, muscle and joint pain, nausea, headaches, insomnia, low mood. No new inflammation. No fever. No lab abnormalities.
- Disease flare: Specific to your condition. Swollen, hot joints in RA. Diarrhea and abdominal pain in IBD. Rash or kidney issues in lupus. Blood tests and imaging will show active disease.
- Adrenal insufficiency: This is an emergency. Dizziness when standing (orthostatic hypotension), low blood pressure, low sodium, low blood sugar, vomiting, confusion. This means your body can’t make cortisol at all. It needs immediate steroid support.
Doctors use a cosyntropin (ACTH) stimulation test to check adrenal function. A cortisol level above 400-500 nmol/L after the test means your adrenals are waking up. Below that? You might need to slow the taper-or temporarily go back up.
How to Make Tapering Easier
Medication alone won’t fix withdrawal. Your body needs support. Here’s what actually works, based on real patient data:
- Movement: Walking 20 minutes a day or doing water-based exercises cuts muscle and joint pain by 42%, according to a Rheumatology Network study. Warm water reduces stiffness without stressing joints.
- Sleep: Aim for 7-9 hours. Poor sleep worsens fatigue and mood swings. One study found patients who maintained good sleep had 55% less severe symptoms.
- Diet: A Mediterranean-style diet-rich in vegetables, fish, nuts, and olive oil-helps stabilize energy and reduce inflammation. Avoid sugar spikes. They make fatigue worse.
- Caffeine: Limit to under 200 mg a day (about one strong coffee). Too much adds to anxiety and disrupts sleep when your body is already stressed.
- Therapy: Cognitive behavioral therapy (CBT) reduced anxiety and depression in steroid withdrawal by 68% in a trial by the American Addiction Centers. Talking through fear and frustration makes a measurable difference.
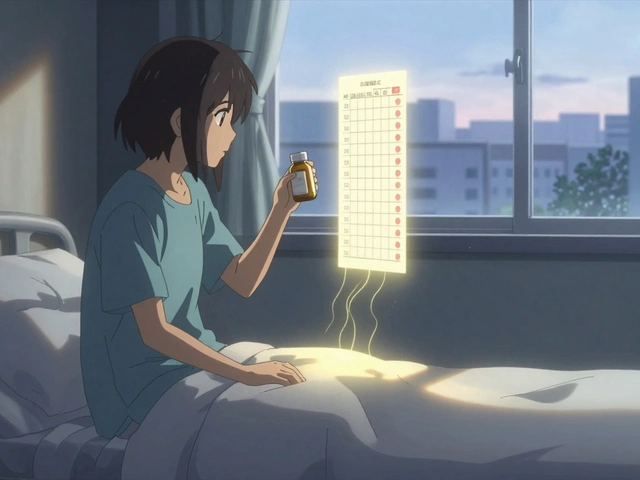
And don’t underestimate the power of routine. Taking your steroid dose in the morning-around 8 a.m.-mimics your body’s natural cortisol rhythm. It helps your adrenals relearn their schedule.
What to Do If Symptoms Hit Hard
Even with the best plan, 22% of patients need to temporarily increase their dose. That’s not failure. It’s smart management.
If you’re feeling worse-fatigue crushing you, pain unbearable, nausea constant-contact your doctor. Don’t guess. Don’t self-adjust. Ask: Is this withdrawal, or is my disease flaring? Your doctor may suggest holding the taper for a week or two, or even bumping up the dose by 2.5 mg temporarily.
Some patients need a longer taper than planned. That’s okay. Recovery isn’t a race. The goal isn’t to get off steroids fast. It’s to get off without wrecking your body.

Red Flags and What to Carry
Always carry a steroid emergency card. It should list your highest prescribed dose and the equivalent in hydrocortisone (usually 20-30 mg). Why? If you get sick with the flu, have an accident, or need surgery, your body can’t ramp up cortisol on its own. You need extra steroids to survive.
Learn to check your orthostatic blood pressure. Sit for a minute, then stand. If your systolic pressure drops more than 20 mmHg, that’s a warning sign of adrenal insufficiency. Call your doctor immediately.
Also, know your limits. If you’re feeling unwell and can’t keep food down, or you’re dizzy and confused, don’t wait. Go to the ER. Say: I’m on a corticosteroid taper and I think I may have adrenal insufficiency. That phrase gets you help fast.
Why So Many People Struggle
Despite clear guidelines, many patients are left to figure this out alone. A survey of Reddit’s r/Prednisone community (over 12,500 members) found that 68% experienced unexpected withdrawal symptoms-even with a prescribed taper. Why? Three big reasons:
- Doctors don’t always explain the plan clearly. 76% of negative reviews mention poor education.
- Tapering schedules vary wildly between specialists. One rheumatologist drops 1 mg weekly. Another drops 2 mg every 10 days. No consistency.
- Psychological stress is ignored. Anxiety and fear of relapse make withdrawal feel worse.
Patients who had coordinated care-primary doctor, endocrinologist, physical therapist, and counselor-were 89% more satisfied with their taper than those who flew solo.
The Future of Tapering
Things are improving. Mayo Clinic rolled out a digital tapering assistant in March 2024. It tracks symptoms, adjusts schedules based on feedback, and alerts doctors when things go off track. In a pilot of 412 patients, it cut complications by 37%.
Researchers are also exploring biomarkers-like the cortisol awakening response in saliva-to predict how fast someone’s HPA axis will recover. Early results show 82% accuracy. Imagine a test that tells you: “You’re ready to drop another 1 mg next week.” That’s the future.
But for now, the best tool is still awareness, patience, and a solid plan. Don’t rush. Don’t ignore symptoms. And don’t let anyone tell you it’s “all in your head.” Your body is relearning how to function without a drug it’s depended on for months or years. That takes time. And it deserves care.
How long does steroid withdrawal last?
Withdrawal symptoms usually last between 2 to 8 weeks, but some people report them for up to 60 days or longer. The duration depends on how long you were on steroids, your dose, and how slowly you tapered. People on long-term therapy (over 12 months) often take 6 to 12 months to fully recover their adrenal function, even after stopping the drug.
Can you stop prednisone cold turkey?
No. Stopping prednisone suddenly after taking it for more than 2-4 weeks can cause adrenal insufficiency, a life-threatening condition. It also triggers severe withdrawal symptoms like extreme fatigue, nausea, muscle pain, and low blood pressure. Always follow a medically supervised taper plan.
What’s the difference between withdrawal and a disease flare?
Withdrawal symptoms are general: tiredness, body aches, nausea, sleep issues, low mood. There’s no new inflammation. A disease flare shows condition-specific signs: swollen joints in rheumatoid arthritis, bloody diarrhea in ulcerative colitis, or a new rash in lupus. Blood tests and imaging help confirm the difference. If you’re unsure, get checked-misdiagnosis happens in 34% of cases.
Do I need blood tests during tapering?
Not always, but they’re important if you’re having symptoms at low doses (below 5 mg). A cosyntropin stimulation test checks if your adrenals are producing enough cortisol. A peak level above 400-500 nmol/L means your HPA axis is recovering. If it’s low, your taper may need to slow down.
Should I take supplements during a steroid taper?
There’s no strong evidence that specific supplements speed up recovery. But supporting your body helps: vitamin D and calcium for bone health (steroids weaken bones), magnesium for muscle cramps, and omega-3s to reduce inflammation. Always talk to your doctor before starting anything new-some supplements can interact with medications.
Can I exercise while tapering off steroids?
Yes, and you should. Gentle movement like walking, swimming, or yoga reduces muscle pain and fatigue. A 2022 study showed 20-minute daily walks improved symptoms by 42%. Avoid intense workouts if you’re feeling weak or dizzy. Listen to your body. Rest when needed, but stay active.
What if I feel fine but my doctor wants me to keep tapering?
Feeling fine doesn’t mean your adrenals are fully recovered. Many people feel okay until they drop below 5 mg, then crash. Stick to the plan. Rushing increases the risk of adrenal insufficiency later. Your doctor’s goal isn’t to make you suffer-it’s to prevent a medical emergency down the line.
Are there alternatives to tapering?
Not really. Tapering is the only safe way to stop long-term corticosteroid use. Some experimental drugs in development aim to speed up HPA axis recovery, but they’re still in early trials. For now, the best approach is a slow, supported taper combined with lifestyle changes and medical monitoring.


OMG this is so real 😭 I tapered from 20mg over 10 weeks and still felt like a zombie for 3 months. My dog started avoiding me because I cried during Netflix. But walking every morning? Game changer. Even 10 minutes helped. My joints stopped screaming. 💪
It’s important to recognize that corticosteroid withdrawal is not merely a side effect-it is a physiological recalibration of the hypothalamic-pituitary-adrenal axis. Many clinicians underestimate the complexity of this process. The body does not reset on a schedule; it resets on its own terms. Patience, not pressure, is the cornerstone of recovery.
I hate how doctors just hand you a taper sheet like it’s a recipe. No one tells you how lonely it feels when you’re too tired to talk to anyone, and your partner thinks you’re being dramatic. I lost my job because I couldn’t get out of bed. And now they say I ‘should’ve tapered slower.’ Like I had a manual.
This is all just Big Pharma’s way of keeping you dependent. Why do you think they don’t want you to stop fast? Because if you could just quit cold turkey and be fine, they’d lose billions. They invented ‘withdrawal symptoms’ to scare you into staying on the drug forever. And now they’re selling you ‘tapering assistants’ like it’s some high-tech miracle? Please. The real cure is detoxing your liver, drinking lemon water, and getting off all pharmaceuticals. I did it. I’m 72 and feel better than my grandkids. They just don’t want you to know the truth.
There’s something deeply human about how our bodies remember what they’ve been through. Corticosteroids don’t just change chemistry-they change your relationship with yourself. You start doubting every ache, every yawn, every mood swing. Is this me? Or is this the drug leaving? The answer isn’t in the labs or the charts. It’s in showing up for yourself, even when you feel broken. Slow is not failure. Rest is not weakness. Recovery isn’t a race-it’s a homecoming.
Have you ever wondered if the ‘HPA axis suppression’ theory is just a cover for the fact that steroids cause permanent damage? I read a whistleblower report from 2021 that said the FDA knew about adrenal atrophy risks since 1998 but buried the data. The ‘taper’ is just damage control. They’re not helping you-they’re managing lawsuits. And now they want you to trust a digital assistant? That’s not medicine. That’s surveillance.
Stop whining. I was on 60mg for 6 months. Tapered in 3 weeks. No problems. You people need to grow up and stop being babies.
I went from 10mg to 0 in 2 weeks. Felt awful. Went back to 5mg. Now doing 1mg every 2 weeks. Still tired but not dying. Walking helps. Sleep more. Don't rush.