Steroid-Induced Osteoporosis Prevention Calculator
This tool helps you understand your risk of steroid-induced osteoporosis and what preventive steps you should take based on your medication regimen and personal factors.
Your Steroid Information
Your Personal Risk Factors
When you’re on long-term steroids-whether for asthma, rheumatoid arthritis, lupus, or another autoimmune condition-you’re not just managing your main illness. You’re also quietly putting your bones at risk. Steroid-induced osteoporosis isn’t a side effect you can ignore. It doesn’t hurt at first. You won’t feel your bones getting weaker. But within months, your risk of breaking a hip, spine, or wrist can jump five to seventeen times higher than someone not on steroids. The good news? You can stop it. And it starts with three simple things: calcium, vitamin D, and bisphosphonates.
Why Steroids Attack Your Bones
Glucocorticoids like prednisone are powerful. They calm inflammation, suppress immune attacks, and save lives. But they also mess with how your bones renew themselves. Your skeleton isn’t static-it’s alive. Every year, old bone is broken down and replaced with new bone. Steroids throw this cycle out of balance.
They shut down bone-building cells called osteoblasts. That means less new bone gets made. At the same time, they wake up bone-eating cells called osteoclasts. More bone gets broken down. The result? You lose bone density fast. Studies show that within 3 to 6 months of starting steroids at 5 mg or more of prednisone daily, bone loss begins. By the end of the first year, up to 12% of people on higher doses will have a spine fracture-often without any fall or injury.
This isn’t just about older people. Even young adults on long-term steroids are at risk. The damage builds silently. That’s why prevention isn’t optional-it’s essential.
The Foundation: Calcium and Vitamin D
Before you even think about drugs, you need the basics. Your bones are made of calcium. And your body needs vitamin D to absorb it. If you’re on steroids, your body doesn’t just need the same amount of calcium and vitamin D as a healthy person-it needs more.
The American College of Rheumatology recommends at least 1,000 to 1,200 mg of calcium every day. That’s about three servings of dairy, or a mix of fortified plant milk, leafy greens, and supplements. If you’re not getting enough from food, a supplement fills the gap. Don’t take it all at once. Your body can only absorb about 500 mg at a time. Split your dose-morning and night.
Vitamin D is even more critical. Steroids interfere with how your body uses it. Experts recommend 600 to 800 IU daily for most people on steroids. But if your blood test shows you’re low-under 30 ng/mL-you’ll need 800 to 1,000 IU daily until you’re back in range. In Australia, where sunlight isn’t always reliable, especially in winter, many people are deficient. A simple blood test can tell you where you stand.
Skipping these two is like trying to build a house without bricks or cement. No drug will work well if your foundation is weak.
Bisphosphonates: The First-Line Defense
If you’re on steroids for more than 3 months and you’re 40 or older-or if you’re younger but already had a fracture-your doctor should recommend a bisphosphonate. These are the most proven, most used, and most cost-effective drugs for preventing steroid-induced bone loss.
Oral bisphosphonates like alendronate (Fosamax) and risedronate (Actonel) are taken once a week. They stick to your bone and slow down the cells that break it down. In clinical trials, alendronate increased spine bone density by 3.7% in one year-while the placebo group lost bone. Risedronate cut the risk of spine fractures by nearly 70%.
But they’re not perfect. You have to take them right. Swallow them with a full glass of water first thing in the morning, before eating or drinking anything else. Stay upright for at least 30 minutes. Lie down too soon, and you risk serious irritation to your esophagus. About 1 in 5 people can’t tolerate them because of stomach upset or heartburn.
That’s where the injectable option comes in: zoledronic acid. Given once a year as a 15-minute IV drip, it’s just as effective as the weekly pills-and far easier to stick with. In one study, patients were 38% more likely to keep taking it after a year. No daily reminders. No upright waiting. Just one visit to the clinic.

When Bisphosphonates Aren’t Enough
Some people need more than a bone protector. They need a bone builder.
If you’ve already had a fracture, your T-score is below -2.5, or you’re on high-dose steroids for more than a year, bisphosphonates might not be enough. That’s where teriparatide (Forteo) comes in. It’s not a blocker-it’s a stimulator. It’s a synthetic version of parathyroid hormone, given as a daily injection under the skin. It tells your body to make new bone, not just preserve old bone.
In a major study, people on teriparatide had a 90% lower risk of new spine fractures than those on alendronate. But it’s expensive-about $2,500 a month compared to $250 for generic bisphosphonates. And you can only use it for two years total. After that, you switch to a bisphosphonate to lock in the gains.
Another option is denosumab (Prolia), given as a shot every six months. It’s very effective at reducing spine fractures-almost 80% lower risk. But if you stop it, you can lose bone fast. So you can’t just quit it cold turkey. You need to transition carefully to another drug.
Who Gets Treatment and When
Not everyone on steroids needs drugs. But too many people don’t get the right care. A 2021 study found that only 1 in 5 eligible patients received bone protection within three months of starting steroids.
Here’s the simple rule: if you’re taking 2.5 mg or more of prednisone (or the equivalent) for 3 months or longer, you should be evaluated. That means a bone density scan (DXA) and a blood test for vitamin D. If you’re 40 or older, you almost certainly need a bisphosphonate. If you’re under 40 but have other risk factors-like smoking, low body weight, or a history of fractures-you still need it.
And if you’re on steroids for life? You need a long-term plan. Bone density should be checked every year. If you lose more than 5% of bone density in a year, it’s time to switch or upgrade your treatment.
Pitfalls and Problems
Even the best treatments have downsides.
Oral bisphosphonates can cause jawbone problems (osteonecrosis), but that’s rare-less than 1 in 10,000 people. Atypical femur fractures are even rarer-about 3 to 50 cases per 100,000 people per year. The risk is so low that the benefits far outweigh it.
But the biggest problem isn’t side effects. It’s forgetting to take the pills. Half to 70% of people stop bisphosphonates within a year. That’s why many doctors now push for the yearly IV option. It’s not just more effective-it’s more reliable.
Also, if you have kidney problems (eGFR under 30), you can’t use oral bisphosphonates. That’s when teriparatide or denosumab become the go-to options.
What Comes Next
The future of steroid-induced osteoporosis treatment is moving toward smarter, personalized care. New drugs like abaloparatide are showing even better bone-building results than teriparatide. Researchers are testing sequences-starting with a bone builder like teriparatide, then switching to a bone saver like zoledronic acid. Early results suggest this combo could give you the strongest bones possible.
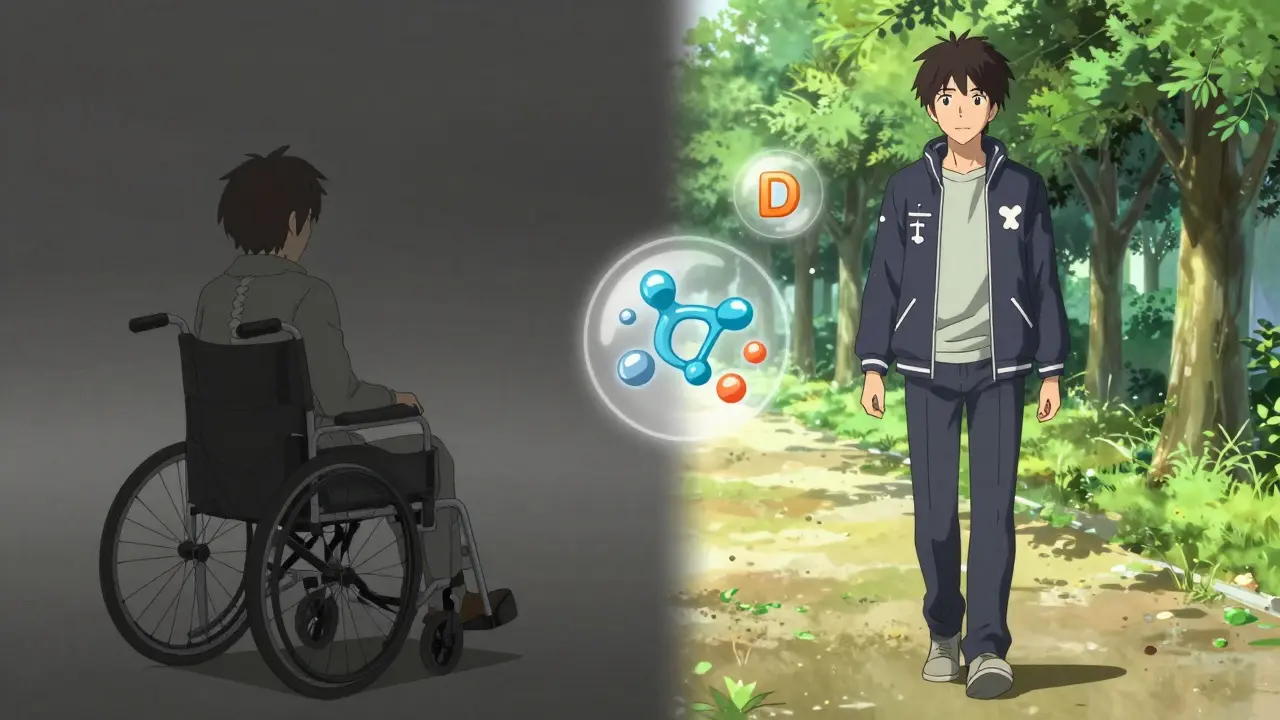
But for now, the answer is simple: if you’re on long-term steroids, don’t wait for a fracture to happen. Get your calcium and vitamin D checked. Ask your doctor about a bone scan. And if you’re at risk, start a bisphosphonate. It’s not glamorous. But it’s the difference between walking normally in your 60s-and ending up in a wheelchair.
Protecting your bones isn’t about being extra careful. It’s about being smart. Steroids save your life. But they don’t have to steal your mobility.
Can I get enough calcium from food alone while on steroids?
It’s very hard. You’d need about 3 to 4 servings of high-calcium foods daily-like milk, yogurt, cheese, sardines, or fortified tofu. Most people don’t eat that much. Plus, steroids reduce calcium absorption. Even if you eat well, you’ll likely still need a supplement to hit the 1,000-1,200 mg daily target.
Do I need to take vitamin D year-round, even in summer?
Yes. In places like Sydney, even in summer, many people don’t get enough sun exposure due to sunscreen use, indoor jobs, or skin cancer concerns. Steroids also make your body less efficient at using vitamin D. Blood tests are the only way to know your level. Most people on long-term steroids need supplements regardless of season.
Are bisphosphonates safe for people with kidney issues?
Oral bisphosphonates like alendronate are not safe if your kidney function is below 30 mL/min (eGFR). For mild to moderate kidney issues (eGFR 30-50), your doctor may lower the dose. If your kidneys are severely impaired, alternatives like denosumab or teriparatide are preferred because they don’t rely on kidney filtration.
How long should I stay on bisphosphonates for steroid-induced osteoporosis?
There’s no fixed time. If you’re still on steroids after 3-5 years, you may need to continue. Some doctors use a "drug holiday" after 5 years if your bone density has stabilized and you’ve stopped steroids-but only if your fracture risk remains low. If you’re still taking steroids, you’ll likely need ongoing treatment. Always discuss this with your doctor before stopping.
Is teriparatide worth the cost?
For high-risk patients-those with prior fractures or very low bone density-it often is. While it costs about 10 times more than generic bisphosphonates, it prevents fractures that can lead to hospitalization, surgery, or long-term care. For someone who’s already broken a bone, the cost of not using it can be far higher than the drug itself.
Can I switch from oral bisphosphonates to the yearly IV shot?
Yes, and many patients do. If you’re struggling with stomach side effects or forgetting pills, zoledronic acid is a great alternative. Your doctor will check your kidney function and vitamin D levels first. You can usually switch directly-no waiting period. The yearly shot is just as effective and much easier to stick with.
What happens if I stop taking steroids but still have low bone density?
You still need treatment. Bone loss from steroids doesn’t reverse just because you stop the drug. Your bone density will continue to decline unless you take action. Even after stopping steroids, you should continue your osteoporosis treatment for at least another year, and often longer, depending on your fracture risk and bone scan results.
Next Steps: What to Do Today
If you’re on steroids and haven’t talked to your doctor about bone health, here’s what to do:
- Ask for a blood test to check your vitamin D level.
- Make sure you’re taking 1,000-1,200 mg of calcium daily, split into two doses.
- Request a DXA bone density scan-especially if you’re over 40 or have other risk factors.
- If your T-score is below -1.5 or you’ve had a fracture, ask about starting a bisphosphonate.
- If you can’t tolerate pills, ask about the yearly IV zoledronic acid.
Don’t wait for a broken bone to act. Steroid-induced osteoporosis is preventable. But only if you start early-and stay consistent.



Just started prednisone for my RA last month. This post saved me from walking into a fracture blind. Already got my D level checked-was at 21. Started 1000 IU daily and 1200 mg calcium split two ways. No more excuses.
Look, I get it. Calcium, vitamin D, bisphosphonates-sounds like a pharmacy commercial. But here’s the real truth: no one tells you how much of a hassle it is to swallow a pill on an empty stomach, stay upright for half an hour, and then pretend you didn’t just ruin your breakfast. I’ve been on this for two years. I’ve missed doses. I’ve forgotten. I’ve lied to my doctor. And yeah, I’m still alive. But my spine? Not so much. I got that compression fracture last winter. Now I’m on the IV drip. It’s easier. But I wish I’d done this right the first time instead of waiting for my body to break down like a cheap lawn chair.
How quaint. You treat osteoporosis like a checklist item: calcium, vitamin D, bisphosphonates-check, check, check. But you ignore the elephant in the room: why are we prescribing steroids for chronic autoimmune conditions in the first place? We’re treating symptoms, not root causes. Why not address gut permeability? Why not test for heavy metals? Why not explore low-dose naltrexone or the Wahls Protocol? You’re all so obsessed with pharmaceutical Band-Aids that you’ve forgotten medicine was once about healing, not just suppressing. And now we have a generation of brittle-boned zombies taking pills they don’t understand, because the system told them to.
As someone from Indonesia who’s been on steroids for lupus for 8 years, I can tell you-this is life or death. In my country, most doctors don’t even know about steroid-induced osteoporosis. I had to research it myself after I fell and broke my wrist. I started taking calcium with vitamin D, and my doctor finally agreed to the yearly IV. Now I’m 42 and still walking. Don’t wait like I did. Ask. Push. Fight for your bones. They’re the only thing holding you up when the meds try to knock you down.
Hey, if you’re reading this and you’re on steroids-you’ve got this. Seriously. It’s not about being perfect. It’s about showing up. Even if you forget your pill once, take it the next day. Even if you skip a vitamin D dose, get outside for 15 minutes. Even if the IV appointment feels like a chore, go. Your future self will thank you. Bone health isn’t glamorous, but it’s the quiet superpower that lets you hug your kids, play with your grandkids, and walk into your 70s without a cane. You’re not just surviving-you’re building a legacy. Keep going.
So we’re told to take calcium like it’s a magic bullet. But if your body’s been chemically neutered by prednisone, does it even matter? Are we just playing whack-a-mole with biology? And what’s the real cost of all this? Not just money-time, anxiety, the daily ritual of pill-popping like some kind of medical monk. I wonder if we’re treating the disease… or just the fear of it.
Yeah, I took the pills. Then I stopped. Then I got the IV. Then I stopped that too. Now I’m 45, have three fractures, and my doctor says I should’ve started earlier. But here’s the thing-I didn’t feel anything. Why should I care? I’m fine. I’m still walking. Maybe I’m just lucky. Or maybe the system scared me into treatment for a problem I didn’t know I had. I’m not mad. Just… tired.
They’re lying. 😈 The pharmaceutical companies made this up to sell drugs. You don’t need bisphosphonates. Just eat bone broth and dance under the moon. 🌙💀 I saw a TikTok that said steroids actually strengthen bones if you take magnesium. 🤯
Let’s not romanticize the IV drip like it’s some elite wellness ritual. Zoledronic acid? It’s a chemical sledgehammer. And yes, it works-but only because it’s brutal. You get flu-like symptoms for 48 hours. Your kidneys get taxed. You pay $1200 out of pocket if your insurance plays hardball. This isn’t prevention-it’s damage control with a side of trauma. And don’t even get me started on the ‘drug holiday’ myth. You think your bones just chill out after five years? Nah. They’re just waiting to collapse when you stop. Welcome to modern medicine: we don’t fix you. We manage the collapse.
Thank you for this. I’ve been scared to ask my rheumatologist about bone scans. I didn’t want to seem ‘difficult.’ But now I’m going in next week. I’m 38, on 7.5 mg prednisone, and I’ve never had a D test. I’m doing it. For me.
THIS. THIS RIGHT HERE. 🙌 I was skeptical too. But after my hip fracture last year, I’m all in. Calcium, D, and the yearly IV. I’m not just surviving-I’m thriving. I’m hiking again. I’m dancing with my wife. You can too. Don’t wait. Start today. Your future self is begging you.