Warfarin: What It Is, How It Works, and What You Need to Know
When you’re prescribed warfarin, a blood-thinning medication used to prevent dangerous clots in the heart, legs, or lungs. Also known as Coumadin, it’s one of the most widely used anticoagulants in the world — but also one of the trickiest to manage safely. Warfarin doesn’t dissolve clots. It stops new ones from forming by blocking vitamin K, which your body needs to make clotting proteins. That’s why even small changes in your diet, other meds, or health can throw your whole system off.
Managing warfarin isn’t just about taking a pill every day. It’s about INR monitoring, a blood test that measures how long it takes your blood to clot. Doctors use this number to adjust your dose — too low, and you’re at risk for a stroke or pulmonary embolism; too high, and you could bleed internally from a minor bump. Most people need testing every few weeks, sometimes even weekly, especially when starting out or changing routines. And because warfarin interacts with so many things — from antibiotics to green vegetables to herbal supplements — keeping track of everything matters. A single change in your kale intake or a new OTC painkiller can send your INR into dangerous territory.
That’s why so many people on warfarin end up in the ER. It’s not because they forgot their pill. It’s because they didn’t know that drug interactions, like mixing warfarin with certain antibiotics or even common cold medicines, can spike bleeding risk. Or that anticoagulant, a broad category of drugs that includes newer options like apixaban or rivaroxaban, might be a better fit for them — simpler, more predictable, and less tied to diet. But if you’re on warfarin, you’re stuck with the routine. You need to know your numbers, your foods, your meds, and your limits.
What you’ll find in these posts isn’t just theory. It’s real advice from people who’ve lived with warfarin — how to handle travel when your INR is unstable, how to avoid dangerous combos with other prescriptions, why some people feel worse switching from brand to generic, and how to talk to your doctor when something feels off. You’ll see how medication safety, dose titration, and even storage practices play into staying healthy on this drug. There’s no magic fix. But with the right info, you can take control — and avoid the mistakes that land others in the hospital.
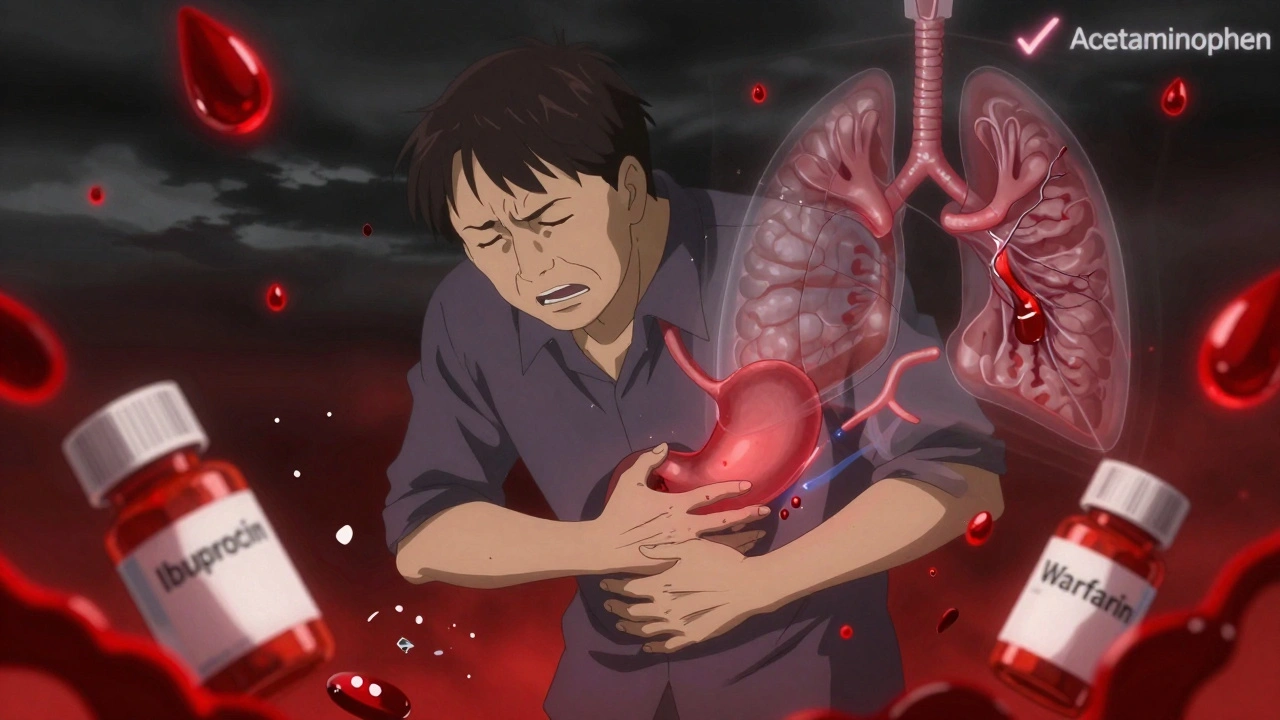
Blood Thinners and NSAIDs: Why This Drug Combo Can Be Life-Threatening
Combining blood thinners with NSAIDs like ibuprofen or naproxen can more than double your risk of dangerous bleeding. Learn why acetaminophen is the only safe OTC pain reliever and what alternatives actually work.