More than 4 in 10 older adults in the U.S. are taking five or more prescription drugs every day. That’s not just common-it’s dangerous. Many of these medications were started years ago for conditions that have changed, or for prevention that no longer matters. Yet they keep getting refilled. No one stops to ask: Do I still need this?
Why Deprescribing Isn’t Just Stopping Pills-It’s Starting Better Care
Deprescribing isn’t about cutting corners. It’s about cleaning up. The term was first defined in 2003 by Australian doctor Michael Woodward to describe the careful, intentional process of stopping medicines that no longer help-or worse, hurt. Today, it’s a standard part of geriatric care. The goal isn’t fewer pills. It’s better health. Less confusion. Fewer falls. More energy. And fewer trips to the ER.Think of it like this: When a doctor prescribes a new drug, they don’t expect it to last forever. They set a goal: lower blood pressure, control pain, prevent infection. Then they check in. Why should stopping be any different? Too often, medications become invisible. They sit in the medicine cabinet, getting refilled year after year, long after the reason they were started is gone.
When It’s Time to Talk About Stopping
There are clear moments when a medication review isn’t just a good idea-it’s urgent.- New symptoms appear. If your loved one suddenly feels dizzy, confused, weak, or has unexplained bruising, it might not be aging-it could be a drug reaction. Sedatives, blood pressure meds, and painkillers are common culprits. One study found that nearly 30% of hospital admissions in seniors are linked to adverse drug events.
- Life expectancy has changed. If someone has advanced dementia, heart failure, or is nearing end-of-life care, preventive drugs like statins or diabetes medications often do more harm than good. These drugs take months or years to show benefit. If someone doesn’t have that time, why keep them?
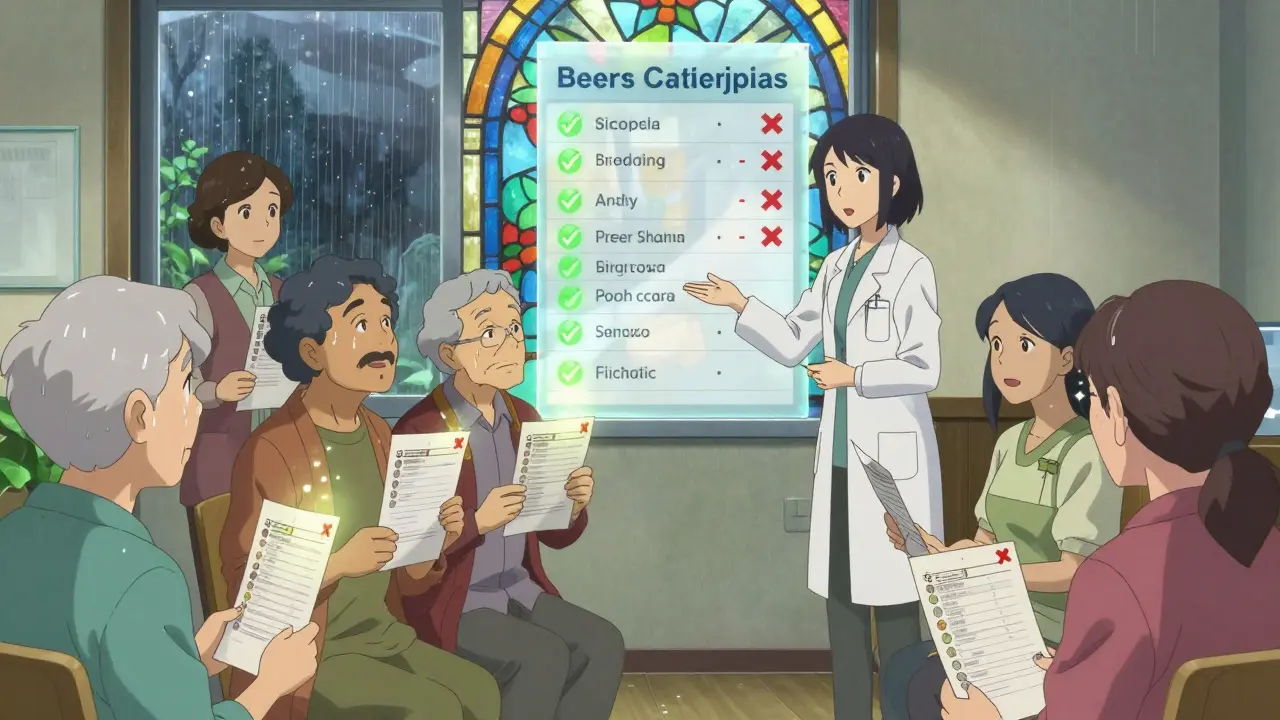
- They’re on high-risk combinations. Some drugs are dangerous together. For example, combining an opioid painkiller with a benzodiazepine for anxiety increases the risk of fatal breathing problems by 40%. The Beers Criteria and STOPP guidelines list these risky pairs-and they’re updated every few years.
- Preventive meds are out of date. A cholesterol pill prescribed at 70 might still be taken at 85. But if the goal was to prevent a heart attack over the next 10 years, and the person’s life expectancy is now 3-5 years, that pill isn’t helping. It’s just adding cost and side effects.
Who Should Be Leading the Review?
This isn’t something to do alone. A medication review should involve a team.A geriatrician or clinical pharmacist is the best person to lead it. They know which drugs are outdated, which ones interact dangerously, and which ones can be safely stopped. Many hospitals and community clinics now offer formal medication reviews. Some pharmacies even run free deprescribing clinics-ask your local pharmacist.
Family members play a key role too. They often notice changes before doctors do: forgetting to take pills, confusion after a new prescription, or a sudden drop in appetite. Don’t wait for the annual checkup. Bring the full list-prescription, over-the-counter, supplements-to any appointment.
And yes, the patient’s voice matters. If someone says, “I don’t want to take this anymore,” that’s not resistance. That’s insight. Their quality of life is the goal-not just ticking boxes on a checklist.

How Deprescribing Actually Works
You can’t just stop a pill overnight. Some drugs need to come off slowly. Others can be cut quickly. Here’s how it’s done right:- List every medication. Include vitamins, herbal supplements, and OTC drugs like antacids or sleep aids. Many seniors don’t realize these count.
- Identify the purpose of each. Why was it prescribed? What’s it supposed to do? If the answer is “I don’t know,” that’s a red flag.
- Check for redundancy. Are two drugs doing the same thing? Is one a newer version of an old one?
- Use the Beers Criteria or STOPP. These are evidence-based lists that flag drugs risky for seniors. For example, long-term use of proton pump inhibitors (PPIs) for heartburn can lead to bone loss and infections. Most people don’t need them beyond 4-8 weeks.
- Stop one at a time. Never cut multiple drugs at once. You need to know which one caused a change-if symptoms improve or worsen.
- Monitor closely. After stopping, watch for 2-4 weeks. Did the dizziness go away? Did sleep get better? Did pain return? Report everything.
Tools like the Deprescribing.org website offer free, step-by-step guides for common drugs-PPIs, sleeping pills, antipsychotics, and more. Each includes a patient handout, a tapering schedule, and what to watch for.
What Happens When You Stop?
Many people fear that stopping a drug will make things worse. But studies show the opposite.One 2022 review found that when seniors had unnecessary medications stopped:
- Adverse drug events dropped by 17-30%
- Hospital readmissions fell by 12-25%
- Quality of life scores improved-especially in energy, sleep, and mental clarity
- There was no increase in deaths or disease flare-ups for the drugs removed
For example, a 78-year-old woman on five blood pressure pills was feeling tired and dizzy. Her doctor cut two that were redundant. Within two weeks, her balance improved. Her energy came back. Her blood pressure stayed controlled.
Another case: a man with dementia on an antipsychotic for agitation. The drug made him sleep 16 hours a day and increased his fall risk. After stopping it, he became more alert, smiled more, and walked without help. His family didn’t realize the drug was the problem.
Barriers-And How to Break Them
Why isn’t this done more often?Doctors don’t always know how. Many were trained to prescribe, not stop. Guidelines focus on starting drugs, not ending them. Pharmacists may refill prescriptions without questioning. And patients? They’re often told, “Just keep taking it.”
Here’s how to push back:
- Ask: “Is this still helping? Can we try stopping it?”
- Bring a printed list of meds to every visit.
- Request a medication review during annual wellness visits-Medicare covers it.
- If your doctor says no, ask for a referral to a geriatric pharmacist.
And don’t be fooled by the myth that “if it’s not broken, don’t fix it.” Many of these drugs are broken-because they’re causing harm.
The Bigger Picture
In 2014, the U.S. spent $30 billion treating adverse drug reactions in seniors. Most of those were preventable. The Centers for Medicare & Medicaid Services now track deprescribing as a quality metric. The World Health Organization has named it a global priority.It’s not about reducing costs. It’s about restoring dignity. It’s about letting someone sleep through the night, walk without fear, or enjoy a meal without feeling foggy. It’s about giving people back control over their own bodies.
Medication reviews aren’t a one-time event. They should happen every time there’s a change-new symptom, new doctor, new hospital stay. Treat every new prescription like a trial. And every refill like a decision.
Can I stop my meds on my own if I think they’re not helping?
No. Stopping some medications suddenly can be dangerous. Blood pressure drugs, antidepressants, seizure meds, and steroids can cause serious withdrawal effects. Always talk to your doctor or pharmacist first. They’ll help you taper safely if needed.
What if my doctor says I need to keep taking all my meds?
Ask why. Request a copy of the Beers Criteria or STOPP guidelines and ask which, if any, of your drugs are flagged. If they’re not familiar with deprescribing, ask for a referral to a geriatric pharmacist or a specialist in老年医学 (geriatric medicine). You have the right to ask for safer care.
Are over-the-counter drugs and supplements included in deprescribing?
Yes. Many seniors take melatonin, sleep aids, antacids, or herbal supplements daily without realizing they can interact with prescriptions or cause side effects. For example, long-term use of antacids like omeprazole increases risk of pneumonia and bone fractures. Always include everything on your list.
How often should a senior have a medication review?
At least once a year. But also after any hospital stay, new diagnosis, or change in function-like falling more often, becoming confused, or losing appetite. Don’t wait for the annual visit. Bring the list anytime you see a provider.
Will stopping meds make my conditions worse?
Not if done properly. Studies show that stopping inappropriate medications doesn’t increase disease risk or death. In fact, people often feel better because they’re not dealing with side effects. The key is targeting drugs that no longer match the person’s current goals, health, or life expectancy.
Next Steps for Families and Caregivers
Start today. Grab the pill organizer. Write down every medication-name, dose, reason, how long they’ve been taking it. Bring it to the next doctor visit. Ask: “Which of these are still necessary?” Then ask: “Which one can we try stopping first?”Deprescribing isn’t a loss. It’s a win. It’s choosing quality over quantity. It’s giving someone back their life, one pill at a time.