Bone Density Risk Calculator
Thyroid-Related Bone Health Risk Assessment
This tool estimates your risk of bone damage based on thyroid condition and other factors mentioned in the article.
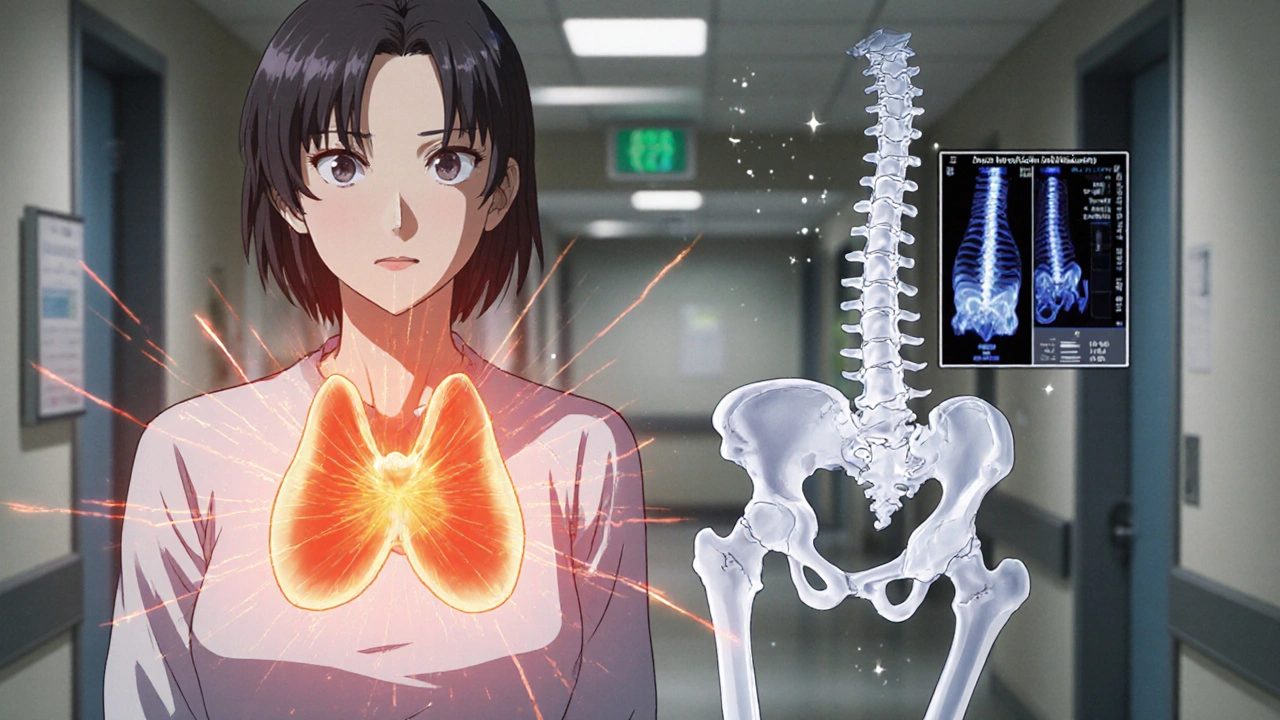
When your thyroid and bones start talking to each other, the conversation can get dangerous. Thyroid disorders throw off hormones that control metabolism, and those hormones also tell bone cells when to build and when to break down. If the balance tips, you can end up with weakened skeletons, frequent fractures, and a whole host of chronic aches.
What Are Thyroid Disorders?
Thyroid disorders are a group of conditions that affect the thyroid gland, a butterfly‑shaped organ at the base of the neck. The gland produces two main hormones - thyroxine (T4) and triiodothyronine (T3) - that regulate metabolism, heart rate, and temperature. The most common forms are hyperthyroidism, where the gland is overactive, and hypothyroidism, where it under‑produces hormones.
Both extremes can ripple through the body, but the impact on bone is often overlooked. Understanding how these hormones interact with bone cells is the first step toward protecting your skeleton.
Bone Damage Explained
Bone damage isn’t just a broken arm. It covers a range of conditions that weaken the mineral matrix - the crystal‑like structure that gives bone its hardness - and disrupt the delicate dance between osteoclasts (cells that break down bone) and osteoblasts (cells that build bone). When this dance goes off‑beat, you can develop osteoporosis, suffer low bone mineral density, or endure frequent fractures.
How Thyroid Hormones Influence Bone Remodeling
Thyroid hormones act like a thermostat for the whole body. In bone, they speed up the activity of osteoclasts, increasing the rate at which old bone is resorbed. At the same time, they boost osteoblasts, encouraging new bone formation. The net result depends on how long the hormone levels stay high or low.
Two key players link thyroid function to bone health:
- Calcium metabolism - thyroid hormones affect how much calcium is absorbed from the gut and how much is excreted in urine.
- Vitamin D - the active form of vitamin D works hand‑in‑hand with thyroid hormones to modulate calcium balance and bone turnover.
When thyroid hormone levels are out of whack, the body’s calcium‑vitamin D axis can go haywire, leading to excessive bone loss.
Hyperthyroidism: A Fast‑Track to Bone Loss
In hyperthyroidism, the thyroid releases too much T3 and T4. This speeds up metabolism but also accelerates bone turnover. Studies from 2023 show that post‑menopausal women with untreated hyperthyroidism have a 30 % higher risk of developing osteoporosis compared to euthyroid peers.
Key mechanisms include:
- Increased osteoclast activity - more bone is broken down each day.
- Reduced calcium absorption - despite high gut calcium, the kidneys dump more of it, lowering serum calcium.
- Suppressed sex hormones - hyperthyroidism can lower estrogen in women, further weakening bone.
Clinically, patients often notice:
- Weight loss despite normal eating.
- Heat intolerance, rapid heartbeat.
- Bone pain, especially in the spine and hips.
If left untreated, the rapid bone turnover leads to a net loss of bone mass, visible on a dual‑energy X‑ray absorptiometry (DXA) scan as a drop in bone mineral density (BMD).
Hypothyroidism: A Subtle Yet Serious Threat
When the thyroid is sluggish - a condition called hypothyroidism - the body’s metabolic rate slows, and bone remodeling slows too. At first glance, slower turnover sounds protective, but the reality is more complex.
Low thyroid hormone levels can reduce the activity of osteoblasts, meaning new bone isn’t formed as efficiently. Over years, this can lead to a gradual thinning of cortical bone and an increased risk of fractures, especially in the hip.
Additional factors that worsen bone health in hypothyroidism:
- Elevated parathyroid hormone (PTH) as the body tries to maintain calcium balance.
- Higher prevalence of vitamin D deficiency - many hypothyroid patients have limited sun exposure or impaired conversion to the active form.
- Weight gain and reduced physical activity, both of which put extra mechanical load on weaker bones.
Long‑term studies from 2022 indicate that men with chronic hypothyroidism have a 15 % higher hip‑fracture rate after age 65 compared to men with normal thyroid function.
Who Is Most at Risk?
Not everyone with a thyroid condition will develop bone damage, but certain groups need extra vigilance:
- Post‑menopausal women - already at risk for osteoporosis, the added hormonal swing can accelerate loss.
- Older adults (≥ 60 years) - bone remodeling slows with age, making the system less able to compensate.
- People on long‑term glucocorticoids - steroids already weaken bone, and thyroid imbalance compounds the effect.
- Individuals with low vitamin D or calcium intake - they lack the raw materials needed for bone repair.
Diagnosing Bone Damage in Thyroid Patients
Early detection hinges on two main tools:
- Bone mineral density testing - A DXA scan measures lumbar spine and hip BMD. A T‑score below -1.0 signals low bone mass; below -2.5 indicates osteoporosis.
- Blood and urine markers - Serum TSH, free T4, and free T3 confirm thyroid status. Calcium, phosphate, 25‑hydroxy‑vitamin D, and PTH levels help assess the calcium‑vitamin D axis.
Advanced labs may also include bone turnover markers such as serum C‑telopeptide (CTX) for resorption and procollagen type 1 N‑terminal propeptide (P1NP) for formation. Elevated CTX in a hyperthyroid patient flags excessive bone loss.

Managing and Preventing Bone Damage
Treatment is two‑fold: control the thyroid and protect the skeleton.
- Thyroid‑specific therapy - Antithyroid drugs (e.g., methimazole) for hyperthyroidism, levothyroxine for hypothyroidism. Achieving a stable euthyroid state often stalls bone loss.
- Calcium and Vitamin D supplementation - Aim for 1,200 mg calcium and 800-1,000 IU vitamin D daily, unless contraindicated.
- Bisphosphonates or denosumab - In patients with confirmed osteoporosis, these medications inhibit osteoclasts and can restore BMD.
- Weight‑bearing exercise - Walking, resistance training, or yoga at least three times a week stimulates osteoblast activity.
- Lifestyle tweaks - Limit alcohol, quit smoking, and keep caffeine intake moderate to protect bone.
Regular follow‑up is key. Repeat DXA scans every 1-2 years and adjust thyroid medication based on TSH targets (0.5-4.5 mIU/L for most adults).
Quick Comparison: Hyper‑ vs. Hypothyroidism Effects on Bone
| Aspect | Hyperthyroidism | Hypothyroidism |
|---|---|---|
| Bone turnover rate | High - osteoclast activity spikes | Low - both resorption and formation slow |
| Typical BMD change | Rapid loss, especially in trabecular bone | Gradual cortical thinning |
| Fracture risk | Elevated, especially vertebral & hip | Increased hip & wrist fractures in older adults |
| Key hormonal driver | Excess T3/T4 | Insufficient T3/T4 |
| Recommended bone meds | Bisphosphonates if BMD < ‑1.0 | Calcium/Vit D + possible bisphosphonate if osteoporosis |
Practical Checklist for Patients
- Get your thyroid function tested yearly if you have a known disorder.
- Schedule a DXA scan within 6 months of diagnosis and repeat as advised.
- Maintain daily calcium (1,200 mg) and vitamin D (800‑1,000 IU) intake.
- Incorporate at least 30 minutes of weight‑bearing activity most days.
- Review medications with your doctor - some antacids and diuretics affect calcium balance.
- Stay hydrated; dehydration can increase urinary calcium loss.
Frequently Asked Questions
Can treating hyperthyroidism reverse bone loss?
Yes, achieving a stable euthyroid state often halts further bone loss. However, any lost bone density may need separate treatment with bisphosphonates or lifestyle changes to rebuild strength.
Do hypothyroid patients need calcium supplements?
Most do, especially if blood tests show low vitamin D or calcium. A daily dose of 1,000-1,200 mg calcium combined with 800-1,000 IU vitamin D supports bone formation while thyroid medication normalizes metabolism.
Is a DXA scan the only way to check bone health?
DXA is the gold standard for BMD, but doctors may also use peripheral ultrasound or quantitative CT for specific regions. Blood markers like CTX and P1NP provide clues about turnover speed, especially in thyroid patients.
Can lifestyle alone protect my bones if I have a thyroid disorder?
Lifestyle is essential but not a substitute for medical treatment. Weight‑bearing exercise, proper nutrition, and avoiding smoking build a stronger base, but you still need thyroid‑specific meds to keep hormone levels in check.
Are there any new drugs on the horizon for bone loss linked to thyroid disease?
Research in 2024 highlighted selective RANKL inhibitors that target osteoclasts without affecting thyroid function. While still in clinical trials, they show promise for patients who cannot tolerate bisphosphonates.
Understanding the tight link between thyroid health and bone integrity empowers you to act early. Keep your thyroid hormones stable, protect your calcium‑vitamin D balance, and give your skeleton the exercise and nutrients it craves. With the right plan, you can keep both systems humming in harmony.



We live in a world where ignoring the silent sabotage of our skeleton by hormonal chaos is almost a moral failing. Thyroid disorders may seem like a niche issue, but they stealthily erode the very framework that holds us upright. When hyper‑thyroidism cranks up bone turnover, it's not just a medical footnote-it's a societal risk of increased fractures and loss of independence. Likewise, hypothyroidism's quiet slowdown can leave elders vulnerable to hip breaks that could have been prevented. It’s our collective duty to demand routine bone density checks for anyone fighting a thyroid imbalance.
The interplay between thyroid hormones and calcium homeostasis is a classic example of endocrine‑skeletal crosstalk. Elevated T3/T4 accelerates osteoclast activity, which can outpace calcium reabsorption in the gut, leading to a net negative balance. Patients should be screened for 25‑hydroxy‑vitamin D levels alongside TSH to catch deficiencies early. A modest supplement regimen-1,200 mg calcium and 800‑1,000 IU vitamin D daily-can mitigate the resorptive surge. Keep an eye on the labs, and the bone will thank you.
It’s infuriating how the medical community often glosses over the bone‑crushing consequences of thyroid imbalance. You’re told the thyroid meds will fix everything, yet months later you’re nursing a stubborn ache in your spine. The relentless cycle of bone loss feels like a secret betrayal. When hyper‑thyroidism robs you of mineral density, it’s not just a number on a DXA; it’s a looming threat of fractures that can shatter lives. I wish more doctors would spotlight this silent danger.
Consider the thyroid as a conductor and bone as the orchestra, each instrument needing the right tempo to stay harmonized. If the conductor runs ahead, the violins (osteoclasts) play too fast, breaking down the melody of bone. If he lags, the cellos (osteoblasts) get lazy and the symphoney thins. It's a delicate dance that reflects deeper philosophic truth about balance in life. Even a slight mistak in dosage can lead to a cacophany of fractures. The key is to keep the rhythm steady by regular monitoring. (typo purposely)
Don’t let thyroid turmoil steal your strength-take charge of your bone health now! With daily calcium, vitamin D, and weight‑bearing moves, you can rebuild what the hormones tried to break. Your skeleton is a powerhouse; fuel it, and it’ll keep you unstoppable.
What they won’t tell you is that big pharma has a vested interest in keeping you on lifelong thyroid medication while your bones quietly crumble. The “standard care” guidelines are riddled with hidden agendas, pushing bisphosphonates that mask the real issue-unchecked hormonal chaos. Every fracture you suffer adds to their profits, and the whispers about selective RANKL inhibitors are being silenced. Stay vigilant, question the narratives, and protect your own skeletal fortress.
Great overview! For anyone managing a thyroid condition, integrating a multidisciplinary plan is essential. Pairing levothyroxine titration with bone‑specific agents like bisphosphonates or denosumab can synergistically restore BMD. Moreover, incorporating biomechanical loading through resistance training enhances osteoblastic activity, creating a positive feedback loop. Remember, adherence to both endocrine and orthopedic recommendations maximizes outcomes.
Regular DXA scans are your best ally.
Oh, because obviously the only people who worry about bone health are the ones who read academic journals for fun. I suppose the rest of us just enjoy living with brittle skeletons, right?
Supporting your bone health is as simple as eating calcium and moving daily it helps strengthen the structure and keeps the thyroid in check also regular testing is key
Norman, let’s set the record straight: dismissing bone health as a niche concern is both inaccurate and dangerous. First, epidemiological data consistently show that thyroid‑induced osteoporosis contributes to a significant percentage of fractures in adults over 60. Second, the cascade begins at the molecular level, where excess T3 amplifies RANKL expression, accelerating osteoclastogenesis. Third, this process is not a trivial footnote; it translates into vertebral compression fractures that can cripple mobility. Fourth, the financial burden on healthcare systems due to fracture‑related hospitalizations is staggering. Fifth, patients with untreated hyper‑thyroidism experience a 30 % higher risk of osteoporosis compared to euthyroid peers. Sixth, even hypothyroid individuals face a stealthy increase in hip fracture incidence, especially men over 65. Seventh, the interplay with vitamin D deficiency compounds these risks, creating a perfect storm of bone loss. Eighth, while bisphosphonates can mitigate resorption, they do not address the underlying hormonal imbalance. Ninth, optimal management therefore requires a dual approach: achieving euthyroidism and supporting bone remodeling through nutrition and exercise. Tenth, weight‑bearing activities like resistance training stimulate osteoblast activity, counterbalancing the catabolic effects of thyroid excess. Eleventh, adequate calcium intake-roughly 1,200 mg per day-provides the necessary substrate for new bone formation. Twelfth, vitamin D supplementation ensures proper calcium absorption, especially in patients with limited sun exposure. Thirteenth, regular monitoring with DXA scans every 1‑2 years enables early detection of BMD declines. Fourteenth, clinicians should incorporate bone turnover markers such as CTX and P1NP to gauge treatment efficacy in real time. Finally, a collaborative care model, involving endocrinologists, rheumatologists, and physiotherapists, is the gold standard for preserving skeletal integrity in thyroid patients. Ignoring these facts does not make them disappear; it merely endangers more lives.
The bone, in its quiet resilience, mirrors the thyroid’s subtle whispers; when one falters, the other feels the echo. Philosophically, balance is not merely a state but a perpetual negotiation between force and form. Thus, safeguarding the skeletal framework becomes an act of honoring the body's deeper harmony.
Yo Albert, they ain’t tellin’ ya that the “simple” labs are rigged to hide the truth. The pharma boys push that calcium‑vit D pill combo just to keep us buying their overpriced brands while they ignore the real fix-resetting hormone signals. Stay woke and demand raw data, not sanitized hype.
Rajesh, you raise an important moral point about collective responsibility. Could you elaborate on how primary care providers might integrate routine BMD screening into thyroid follow‑up visits without overburdening the system? Your insight would be valuable for implementing practical guidelines.
Matthew, your enthusiasm is commendable, but the reality is far more nuanced than a three‑step checklist. First, calcium absorption varies dramatically with age, gastrointestinal health, and even genetic polymorphisms, so a one‑size‑fits‑all dosage is naive. Second, relying solely on weight‑bearing exercise overlooks the need for progressive overload and periodization to truly stimulate osteogenesis. Third, bone‑specific pharmacotherapy must be individualized based on DXA T‑scores and turnover markers, not just “feel‑good” motivation. In short, a comprehensive, data‑driven protocol supersedes generic pep talks.