People living with HIV are living longer than ever. But with that longevity comes a new challenge: managing heart disease risk. Statins, the go-to drugs for lowering cholesterol, are often needed. But combining them with HIV medications isn’t as simple as popping two pills. Some combinations can cause dangerous muscle damage, even life-threatening rhabdomyolysis. The key isn’t avoiding statins-it’s choosing the right one, at the right dose, and knowing what to watch for.
Why HIV Meds and Statins Don’t Always Mix
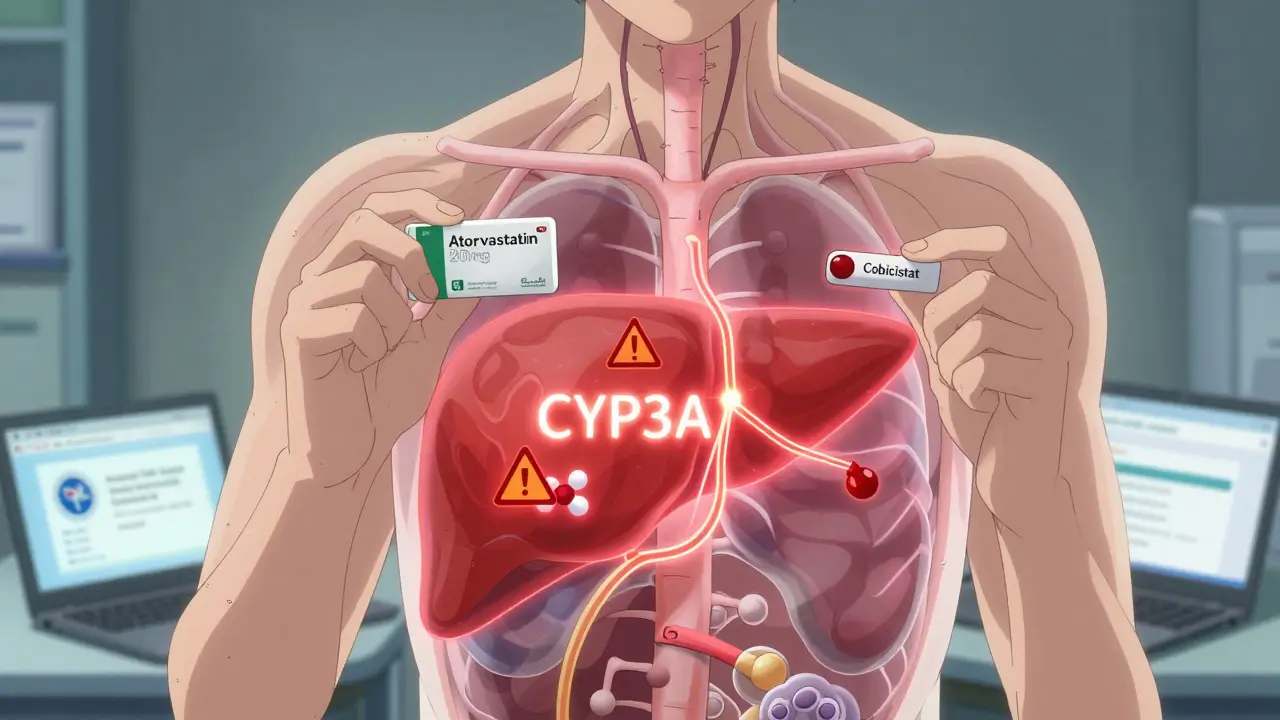
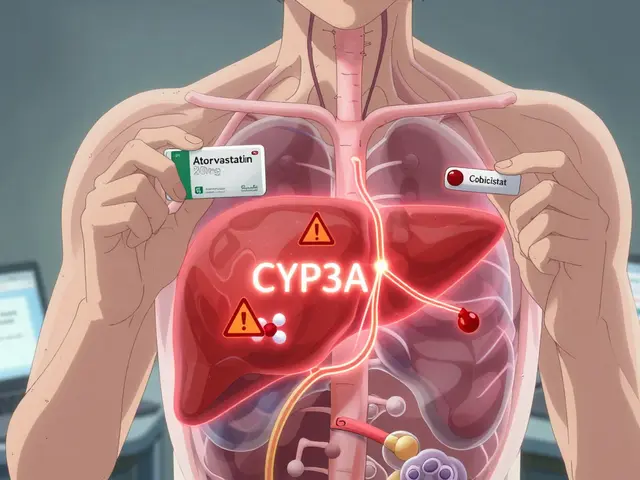
The problem starts in your liver. Both HIV medications and statins are broken down by the same enzymes-mainly CYP3A4-and transported by the same proteins in your bloodstream. Some HIV drugs, especially those with cobicistat or ritonavir as boosters, shut down these enzymes like a circuit breaker. That means the statin doesn’t get cleared from your body the way it should. Instead, it builds up to levels 200% to 300% higher than normal. That buildup doesn’t just raise your risk of side effects-it turns a common complaint like muscle soreness into a medical emergency. Rhabdomyolysis, where muscle tissue breaks down and floods your kidneys with toxic proteins, can lead to kidney failure. The FDA issued clear warnings in 2016: never mix simvastatin or lovastatin with any boosted HIV regimen. The risk isn’t theoretical. Studies show these combinations can spike statin levels by up to 20 times.Statins You Must Avoid Completely
If you’re on any HIV regimen with cobicistat (like Symtuza or Prezcobix) or ritonavir (like Kaletra or Norvir), these two statins are off-limits:- Simvastatin (Zocor)
- Lovastatin (Mevacor)
Safe Statin Options and Their Limits
Good news: you still have choices. Not all statins are created equal when it comes to HIV drug interactions. Here’s what works, and how much you can take:1. Atorvastatin (Lipitor)
This is the most commonly used statin in people with HIV. But even here, you need to be careful. If you’re on darunavir/cobicistat, the maximum dose is 20 mg daily-not 40 mg, as some might assume. That’s the official label limit in the U.S. Even at 20 mg, your doctor should monitor you closely, especially if you’re over 65 or have kidney issues.2. Rosuvastatin (Crestor)
Rosuvastatin is another solid option, but it’s not immune to interactions. With ritonavir-boosted regimens, don’t exceed 10 mg daily. The FDA and University of Liverpool’s drug interaction database agree on this cap. At higher doses, exposure can triple, increasing muscle toxicity risk.3. Pitavastatin (Livalo)
This one stands out. Pitavastatin is metabolized differently-mostly by glucuronidation, not CYP3A4. That means it has the fewest interactions with HIV drugs. It’s often the top pick for people on boosted regimens. No dose restrictions are needed with most ART, and studies show it lowers LDL cholesterol just as well as other statins. The catch? It’s more expensive and not always covered by insurance.4. Pravastatin (Pravachol)
Pravastatin is another low-risk option. It’s not processed by CYP3A4 at all, so it’s safe with cobicistat and ritonavir. But it’s less potent than atorvastatin or rosuvastatin, so you might need a higher dose (40-80 mg) to reach your cholesterol goal. It’s also more likely to cause stomach upset in some people.5. Fluvastatin (Lescol)
Fluvastatin is metabolized by CYP2C9, which means it’s mostly safe from CYP3A4 interactions. But if you’re on ritonavir, exposure can still rise by about 2-fold. Use it cautiously, and stick to lower doses (20-40 mg). It’s not first-line, but it’s a useful backup if others aren’t an option.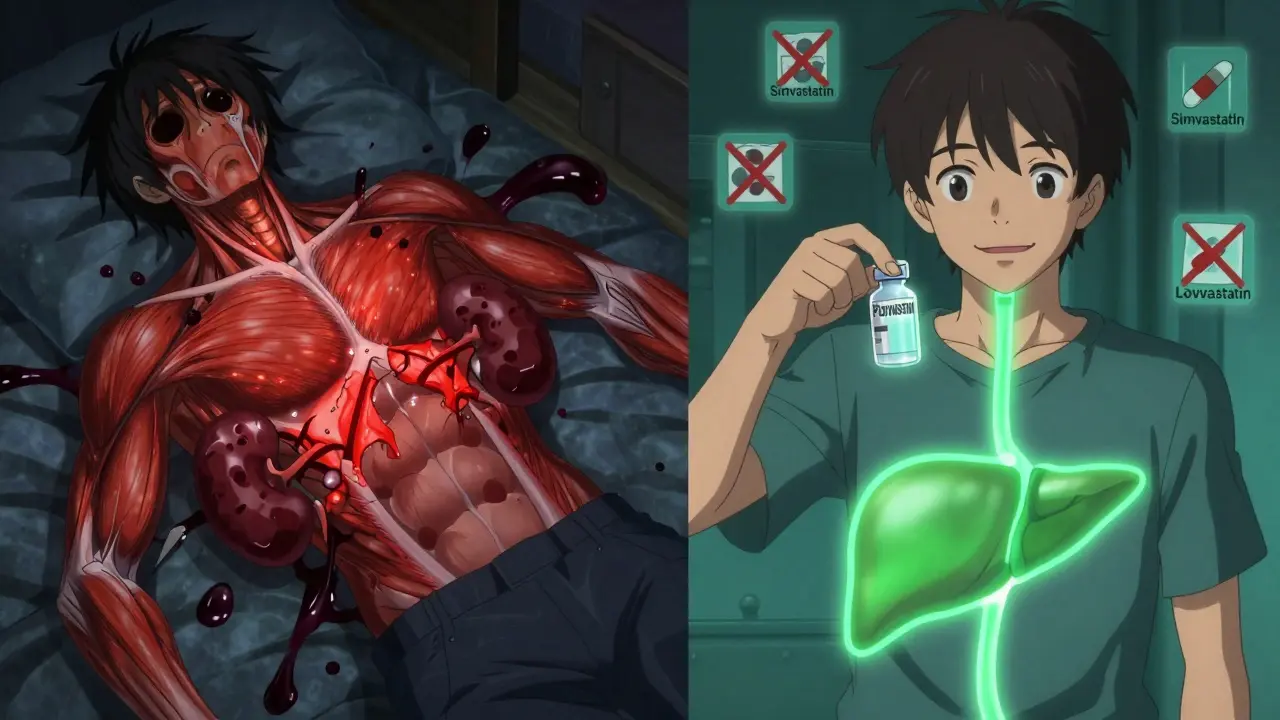
What About Newer HIV Drugs?
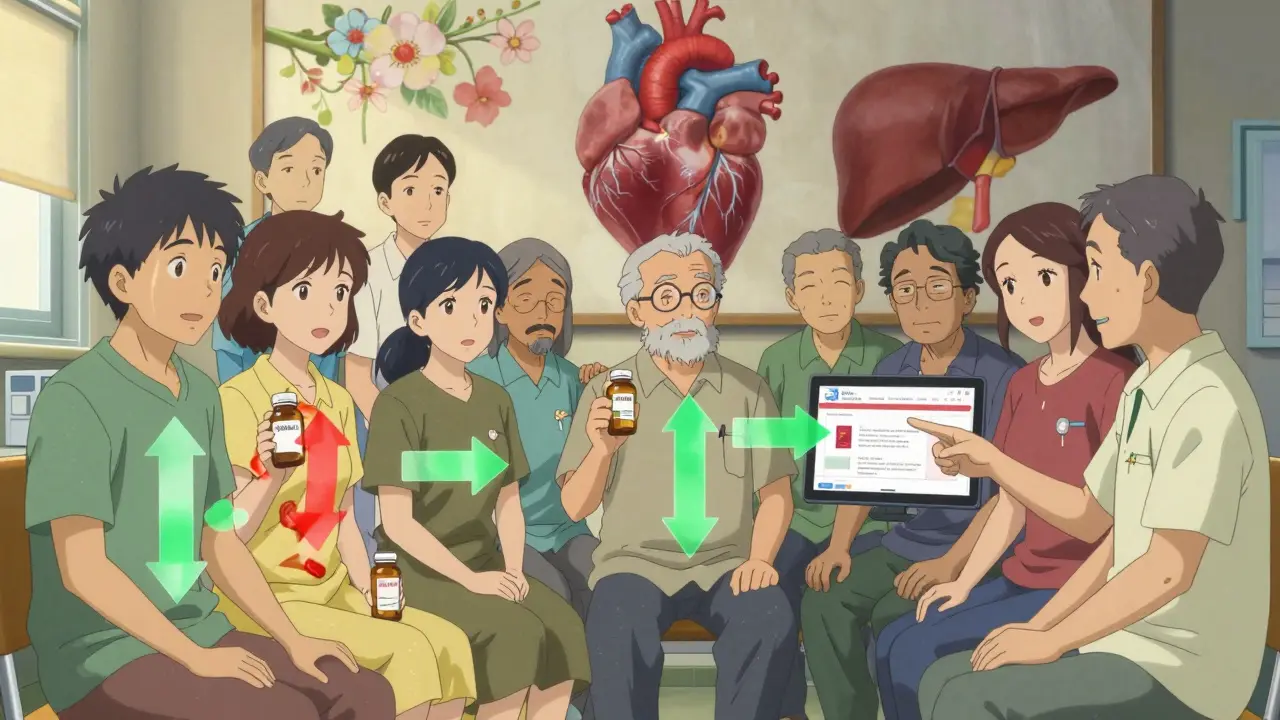
The landscape changed dramatically with integrase inhibitors. Drugs like dolutegravir and bictegravir (found in Triumeq, Biktarvy, and Dovato) don’t significantly affect CYP3A4. That means if you’re on one of these regimens, you can usually take standard doses of atorvastatin, rosuvastatin, or even pitavastatin without dose adjustments. This is a big deal. Many people now start HIV treatment with these newer drugs because they’re simpler, more effective, and easier to combine with other medications. If you’re on one, talk to your doctor about whether you can use a higher statin dose than previously allowed. You might be able to reach your cholesterol target faster and with fewer side effects.What Else Could Make Things Worse?
It’s not just HIV meds and statins. Other common drugs can pile on the risk:- Calcium channel blockers like felodipine or verapamil-often used for high blood pressure-are also broken down by CYP3A4. Using them with a statin and a boosted HIV drug? Triple threat.
- Gemfibrozil, a triglyceride-lowering drug, should be avoided entirely. It increases statin toxicity by interfering with muscle clearance. Fenofibrate is a safer alternative.
- Red yeast rice supplements contain natural statins and can be just as dangerous as prescription ones when mixed with HIV meds.
- Alcohol and grapefruit juice can also raise statin levels. Avoid grapefruit completely if you’re on any statin with HIV treatment.
Monitoring: What Your Doctor Should Check
Even with the right statin and dose, you need monitoring. Here’s what to expect:- Baseline blood tests: Creatine kinase (CK) to check for muscle damage, liver enzymes, and kidney function before starting.
- Follow-up at 4-6 weeks: Repeat CK and liver tests after starting or changing dose.
- Annual checks: Even if you feel fine, get tested yearly.
- Watch for symptoms: Unexplained muscle pain, weakness, or dark urine? Call your doctor immediately. Don’t wait.
What to Do If You’re Currently on a Risky Combination
If you’re on simvastatin or lovastatin with any boosted HIV regimen, stop taking it immediately. Don’t wait for your next appointment. Contact your HIV provider or pharmacist right away. They’ll switch you to a safer statin-usually pitavastatin or pravastatin-and adjust your dose. Many people don’t realize they’re on a dangerous combo because their primary care doctor and HIV doctor aren’t communicating. That’s why it’s critical to bring your full medication list-prescription, over-the-counter, and supplements-to every appointment. Even a simple antacid like cimetidine can interfere.The Best Tool You Don’t Know About
There’s a free, trusted resource that every doctor and patient should use: the University of Liverpool HIV Drug Interactions Checker. It’s updated monthly by a global team of experts and contains over 98,000 interaction records. You can type in your exact HIV meds and statin, and it tells you:- Is this combo safe?
- What’s the maximum safe dose?
- Are there alternatives?
Bottom Line: You Can Still Take Statins Safely
HIV and statins don’t have to be a conflict. The key is knowing which statins are safe, what doses to use, and how to monitor for problems. Avoid simvastatin and lovastatin completely. Pitavastatin and pravastatin are your safest bets. Atorvastatin and rosuvastatin work too-but only at reduced doses. Newer HIV drugs like bictegravir make things easier. Don’t skip statins because you’re afraid. Cardiovascular disease is the leading cause of death in people with HIV over 50. Statins save lives. But they must be chosen and used with precision. Talk to your care team. Use the Liverpool checker. Report any muscle pain. Your heart-and your muscles-will thank you.Can I take atorvastatin with my HIV meds?
Yes, but only if you’re not taking simvastatin or lovastatin. If your HIV regimen includes cobicistat or ritonavir, the maximum safe dose of atorvastatin is 20 mg per day. If you’re on an integrase inhibitor like bictegravir or dolutegravir, you can usually take standard doses up to 80 mg. Always confirm with your doctor or use the University of Liverpool’s HIV Drug Interactions Checker.
Is pitavastatin the best statin for people with HIV?
Pitavastatin is often the top choice because it’s metabolized differently and has the fewest interactions with HIV medications. It doesn’t rely on CYP3A4, so it’s safe with cobicistat and ritonavir without dose limits. It’s also effective at lowering LDL cholesterol. The main downside is cost-it’s more expensive than generic statins like atorvastatin or pravastatin, and insurance coverage can be limited.
Why can’t I take simvastatin with HIV meds?
Simvastatin is broken down by the CYP3A4 enzyme, which is strongly blocked by HIV drugs like cobicistat and ritonavir. This causes simvastatin levels to spike up to 20 times higher than normal. That dramatically increases the risk of rhabdomyolysis-a condition where muscle tissue breaks down, releasing toxins that can cause kidney failure. The FDA and global health guidelines strictly prohibit this combination.
Do I need to stop statins before starting HIV treatment?
No, you don’t need to stop statins entirely. But you must switch to a safe one before or at the same time you start HIV treatment if you’re on a boosted regimen. If you’re currently taking simvastatin or lovastatin, your provider will switch you to pitavastatin, pravastatin, or a lower dose of atorvastatin or rosuvastatin. Never stop statins without medical advice-uncontrolled cholesterol is also dangerous.
What should I do if I feel muscle pain while on statins and HIV meds?
If you experience unexplained muscle pain, weakness, or dark urine, contact your doctor immediately. These could be early signs of rhabdomyolysis. Don’t wait for your next appointment. Your doctor will likely order a blood test for creatine kinase (CK) and kidney function. If levels are high, your statin may need to be stopped or switched. Never ignore these symptoms-even if they seem mild.

Wow, someone actually wrote a responsible article about this. Most people just panic and stop statins entirely. Honestly, it’s about time someone laid out the facts without fearmongering. I’ve been on Biktarvy and atorvastatin for 3 years at 40mg-no issues. Doctors need to stop treating HIV patients like they’re made of glass.