Swelling in your hands or feet might seem like a minor annoyance-maybe you wore tight shoes, or you stood too long. But if it shows up after starting a new medication, it could be your body’s warning sign. About 5 to 10% of people on certain drugs experience this kind of swelling, and for some, it’s a signal that something more serious is going on. You don’t need to wait until it gets worse. Knowing when to call your doctor can prevent complications, hospital visits, or even life-threatening issues.
What Causes Swelling from Medications?
Not all swelling is the same. Two main types come from medications, and they look and feel different.
The first kind is vasodilator-induced edema. This happens with drugs like amlodipine (a common blood pressure medicine), nitrates, or gabapentin. These medications relax your blood vessels to lower blood pressure or ease nerve pain. But when the vessels widen too much, fluid leaks into your tissues-especially in your ankles and feet. It’s usually symmetrical, meaning both feet swell at the same time. You’ll notice it gets worse as the day goes on, and it improves after lying down overnight. Studies show up to 15% of people taking 10 mg of amlodipine daily develop this kind of swelling.
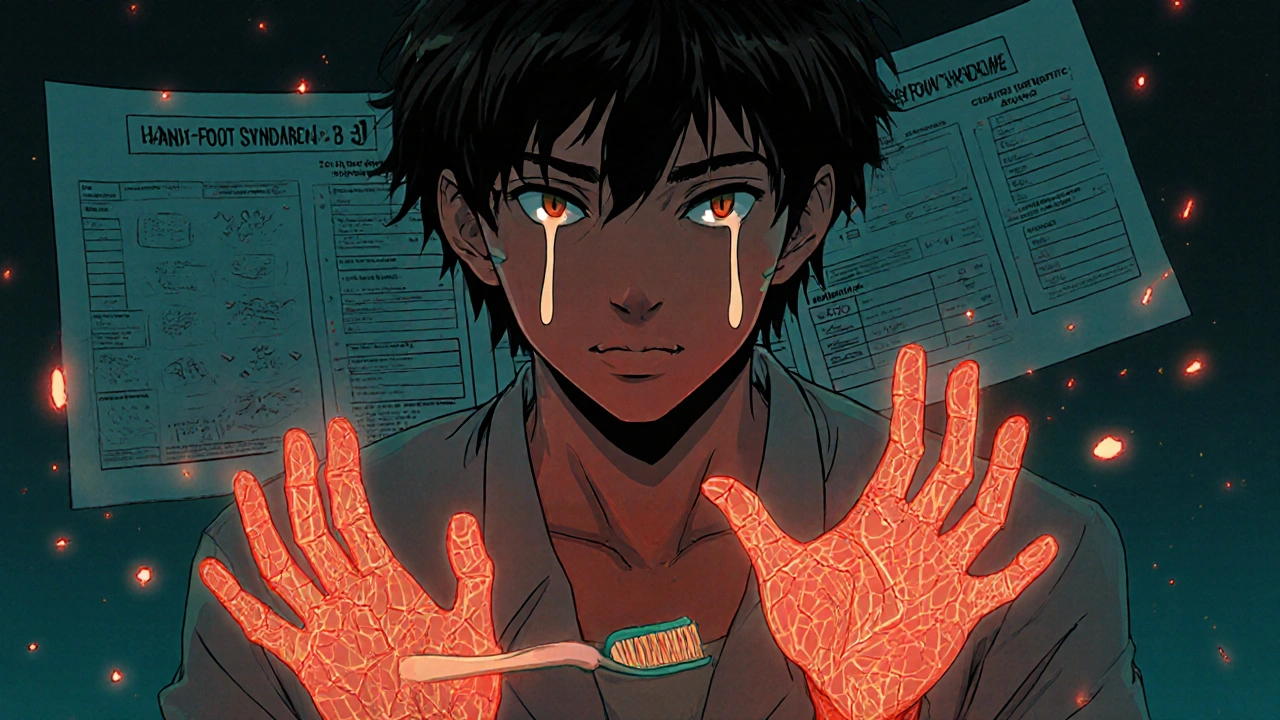
The second kind is hand-foot syndrome (also called palmar-plantar erythrodysesthesia). This one hits the palms of your hands and soles of your feet. It’s most common with chemotherapy drugs like capecitabine, where up to 60% of patients experience it. Symptoms include redness, tingling, numbness, peeling skin, and sometimes painful blisters. Unlike regular swelling, this isn’t just fluid-it’s inflammation from the drug damaging skin cells. Grade 2 or higher can make it hard to hold a toothbrush, open a jar, or walk without pain.
Other medications can cause swelling too. NSAIDs like ibuprofen, steroids like prednisone, and diabetes drugs like pioglitazone can make your body hold onto salt and water. This leads to puffiness in your legs, hands, or even around your eyes. The key is timing: if swelling starts within 72 hours of beginning a new drug, there’s a 78% chance it’s caused by the medication.
When Swelling Is a Red Flag
Not every bit of puffiness needs an emergency room visit. But some signs mean you should call your doctor today.
- One-sided swelling (only one foot or hand) could mean a blood clot. Deep vein thrombosis (DVT) can lead to a pulmonary embolism-this is life-threatening.
- Chest pain, shortness of breath, or rapid heartbeat along with swelling could signal heart failure. Your heart isn’t pumping well, and fluid is backing up.
- Rapid weight gain-more than 2 pounds in 24 hours or 5 pounds in a week-is a clear sign your body is holding too much fluid.
- Skin changes like open sores, blisters, black or purple discoloration, or fever mean the swelling has turned into tissue damage. This is especially critical with hand-foot syndrome.
- Reduced urine output (less than 500 mL per day) suggests your kidneys aren’t working right. Many swelling-causing drugs affect kidney function.
For hand-foot syndrome, guidelines from the American Society of Clinical Oncology say to contact your oncologist immediately if you have Grade 3 symptoms: more than half of your palms or soles affected, pain that stops you from doing basic tasks like dressing or eating, or open wounds. Don’t wait for it to get worse.
What to Do Before You Call
Before you pick up the phone, take a few quick steps. They won’t fix the problem, but they’ll help your doctor diagnose it faster.
- Write down when the swelling started and which medication you began around that time.
- Take a photo of the swollen area. Swelling changes through the day-photos help track progression.
- Check your weight daily. If you’ve gained more than 2 pounds in a day, note it.
- Stop taking NSAIDs or salt-heavy foods temporarily. These can make swelling worse and confuse the picture.
- Elevate your feet for 30 minutes, three times a day. If it helps, it supports the idea that it’s fluid retention.
Don’t try to self-diagnose. Even if you think it’s "just" from amlodipine, other drugs you’re taking could be interacting. Many patients on multiple medications don’t realize one drug is masking the side effect of another.
How Doctors Handle It
Your doctor won’t just tell you to "take a pill and call me in the morning." They’ll look at your full list of medications, your heart and kidney function, and how severe the swelling is.
For calcium channel blocker swelling, the most common fix is switching to a different blood pressure medicine-like an ACE inhibitor or ARB. Studies show 85% of patients see improvement within two weeks after switching. Sometimes, adding a low-dose ACE inhibitor helps reduce the swelling without changing the main drug. Compression stockings (20-30 mmHg) can reduce swelling by 40% in some cases.
For hand-foot syndrome, the first step is almost always reducing the chemotherapy dose. Some oncologists pause treatment for a week to let skin heal. Topical treatments like urea cream or moisturizers help some people, but evidence is mixed. Vitamin B6, often suggested online, doesn’t consistently work-studies show no real benefit. Arnica gel showed promise in one small study, but it’s not standard care.
For swelling from NSAIDs or steroids, cutting back or switching to a different pain reliever often helps. Diuretics (water pills) are sometimes used, but only if your kidneys are okay. Taking them without checking kidney function can cause more harm.
What Doesn’t Work (And Why)
There are a lot of home remedies floating around. Most don’t help-and some can delay real treatment.
Drinking more water won’t flush out the swelling. If your body is holding fluid because of the drug, extra water just adds to the problem.
Massaging your feet might feel good, but if you have a blood clot, it can break it loose. Don’t do it without medical clearance.
Herbal supplements like dandelion or parsley are sometimes touted as natural diuretics. But they’re not regulated, can interact with your meds, and haven’t been proven to help drug-induced swelling.
And yes, you might hear that "it’s normal"-especially with chemo or blood pressure drugs. But here’s the truth: 55% of patients in one survey waited too long to call their doctor because they thought swelling was "just part of the process." That delay led to preventable complications in nearly 1 in 5 cases.
Prevention and Long-Term Outlook
Some swelling can be avoided. Starting amlodipine at 2.5 mg instead of 10 mg cuts swelling risk by 60%. For chemotherapy patients, using urea cream on hands and feet twice daily before symptoms start can reduce hand-foot syndrome by 25%.
Education matters. Patients who get clear instructions on what swelling looks like and when to act are 3.2 times more likely to reach out early. That’s huge. Early action means less pain, fewer missed treatments, and better outcomes.
The good news? Most cases resolve. Of those who get the right care, 89% see swelling go away within four weeks. But 11% develop chronic swelling that needs ongoing management-like compression therapy or physical therapy.
One patient on Reddit described "sock marks that lasted all day" from pregabalin. Another switched from amlodipine to losartan and had complete resolution in five days. It’s not hopeless. But it does require action.
Final Checklist: When to Call Your Doctor
Keep this simple list handy. If even one of these applies, call your doctor now:
- Swelling started within 3 days of starting a new medication
- It’s only on one side
- You gained more than 2 pounds in 24 hours
- You have chest pain, trouble breathing, or dizziness
- Your skin is blistered, cracked, or discolored
- You can’t walk, hold objects, or do daily tasks because of pain
- You’re urinating less than usual
If none of these apply but the swelling is new and bothering you? Still call. You know your body best. A quick call could save you from weeks of discomfort-or worse.
Is hand and foot swelling from medication dangerous?
It can be. While mild swelling from drugs like amlodipine is common and usually not dangerous, sudden or severe swelling can signal serious problems like heart failure, blood clots, or kidney issues. Hand-foot syndrome from chemotherapy can lead to skin breakdown and infection if ignored. Always get it checked.
How long does medication-induced swelling last?
It depends on the cause and how quickly you act. Most cases improve within 2 to 4 weeks after stopping or adjusting the medication. If swelling persists beyond a month, it may be chronic and need long-term management like compression therapy or lifestyle changes.
Can I take a diuretic to reduce the swelling?
Only if your doctor recommends it. Diuretics can help with fluid retention, but they can also strain your kidneys or throw off your electrolytes-especially if you’re on blood pressure or heart meds. Never take a water pill without medical advice.
Does salt make swelling worse?
Yes. Sodium causes your body to hold onto water. If your medication is already making you retain fluid, eating salty foods makes swelling worse. Limiting sodium to under 2,300 mg per day can reduce swelling by 20-25%.
Should I stop taking the medication if I notice swelling?
No-not without talking to your doctor first. Stopping a blood pressure or cancer drug suddenly can be dangerous. Your doctor may adjust the dose, switch you to another drug, or add a treatment to reduce swelling. Never make changes on your own.
Can hand-foot syndrome go away on its own?
Mild cases (Grade 1) may improve if you reduce activity and use moisturizers. But moderate to severe cases (Grade 2 or higher) usually require dose reduction or treatment pause. Without intervention, symptoms can worsen and lead to infection or treatment delays.
What’s the most common drug that causes foot swelling?
Amlodipine, a calcium channel blocker used for high blood pressure, is the most common culprit. Up to 15% of people taking 10 mg daily develop noticeable swelling in their ankles and feet. Other common offenders include nifedipine, gabapentin, and pioglitazone.
Is swelling from medication more common in older adults?
Yes. Older adults are more sensitive to fluid retention due to reduced kidney function and slower metabolism of drugs. They’re also more likely to be on multiple medications, increasing the risk of interactions. About 25% of adults over 65 on calcium channel blockers develop swelling.
Next Steps
If you’re currently taking a medication and notice swelling, don’t ignore it. Write down the details: when it started, how bad it is, and what else you’re taking. Call your doctor or pharmacist. If it’s after hours and you have red flag symptoms-chest pain, one-sided swelling, trouble breathing-go to urgent care or call 911.
Medications save lives. But they can also cause side effects that need attention. You’re not overreacting if you speak up. Early action keeps you safe, keeps your treatment on track, and helps you feel like yourself again.



Okay but have y’all noticed that ALL modern meds are just slow poison disguised as solutions? I mean, amlodipine? That’s just calcium channel blocker magic trickery-your body’s like ‘uhhh why are my ankles drowning?’ and the doc says ‘it’s normal’ like we’re pets in a lab. I’ve been on 5 meds since 2020 and my feet look like inflated balloons at a kid’s birthday. They call it ‘edema’ like it’s a fancy spa treatment. Nope. It’s pharmaceutical gaslighting. 🤡
Big respect for laying this out so clearly. I’ve seen friends ignore foot swelling because ‘it’s just water retention’-until they ended up in ER with a DVT. The part about one-sided swelling being a red flag? That’s CRITICAL. I’m sharing this with my mom who’s on amlodipine. She thinks her ‘puffy ankles’ are just aging. Time to get her to the doc.
There’s a critical error in your characterization of hand-foot syndrome. It’s not merely ‘inflammation from drug-induced skin cell damage’-it’s a microvascular toxic reaction mediated by topoisomerase inhibition and reactive oxygen species accumulation, particularly with capecitabine metabolites. The clinical severity correlates with cumulative dose and pharmacokinetic variability due to DPD enzyme polymorphisms. Topical urea helps by enhancing epidermal hydration and barrier repair, not ‘just moisturizing.’ Also, vitamin B6 trials were underpowered; recent meta-analysis (JCO 2023) shows no benefit over placebo. Don’t let anecdotal Reddit posts mislead patients.
Wait… so you’re telling me Big Pharma doesn’t WANT us to know this? 😳 I just read that 85% of people who switch from amlodipine to ARBs get better… but why aren’t doctors telling us this? Are they getting kickbacks? Is this why my cousin’s kidney failed after 3 years on lisinopril? I’ve been researching this for 11 months now and I think this is all part of a global water retention control program. They need us bloated so we buy more meds. I’ve got screenshots. DM me.
I’ve been on gabapentin for 4 years… and yes, my feet swell every afternoon. I elevate them. I wear compression socks. I cut salt. I’ve tried everything. I didn’t realize it was the drug until I read this. I’m calling my neurologist tomorrow. Thank you. Seriously. This is the first time someone explained it without sounding like a textbook. 🙏
You got this. Seriously. Swelling isn’t ‘just part of getting older’ or ‘normal side effects.’ You’re not being dramatic-you’re being smart. Call your doctor. Take a photo. Write it down. You’re already ahead of 90% of people who wait until they can’t walk. I believe in you. You’re doing great.
AMERICA: We’re so advanced we can send robots to Mars… but we can’t fix a simple drug side effect without 17 pills and a 3-month wait? Meanwhile, in Germany, they prescribe lower doses and monitor electrolytes weekly. In India, they use turmeric paste. Here? We just say ‘take a diuretic’ and hope for the best. We’re not healthcare-we’re pharmaceutical roulette.
Okay but what if the swelling is actually a sign you’re too healthy? Like… your body’s rejecting the corporate medicine machine? I’ve been off all meds for 8 months and my feet are smaller than they were in college. Coincidence? I think not. The system wants you bloated, doc-hopping, and dependent. You’re being manipulated. Wake up.
Let’s get tactical. If you’re on chemo and getting HFS? You’re not ‘just’ getting side effects-you’re in a metabolic war zone. Your keratinocytes are under oxidative siege. Proactive prophylaxis = urea 10% BID + ice packs during infusion + avoid tight shoes. No, coconut oil won’t help. No, you don’t need to ‘detox.’ You need protocol. This isn’t yoga-it’s oncology. Get your nurse on the line before it’s Grade 3. Your chemo schedule depends on it.
This is exactly the kind of info we need more of. I’ve had patients quit their meds because they thought swelling was ‘normal’-and then their BP spiked or their cancer treatment got delayed. You’re not overreacting. You’re being responsible. Keep advocating for yourself. And if your doctor brushes you off? Find a new one. Your health isn’t negotiable.
my aunt had this with pioglitazone. she thought it was just her feet ‘getting bigger’ from sitting too much. then she gained 8 lbs in 4 days. she went to the ER thinking she had a heart attack. turned out it was the diabetes med. they switched her to metformin and boom-swelling gone in 10 days. why don’t they warn us about this stuff BEFORE we start the meds??
As a pharmacist in Mumbai, I see this daily. Elderly patients on amlodipine + NSAIDs + diuretics? Swelling is inevitable. But they never connect the dots. We need better counseling-not just handing out scripts. I’ve started giving printed one-pagers to patients: ‘When your socks leave marks all day, it’s not aging-it’s a red flag.’ Simple. Visual. Effective. We need more of this in primary care.
i had this with prednisone… my hands swelled so bad i couldnt hold my coffee cup. i thought it was just ‘steroid puffiness’… but then i realized i was gaining 3 lbs a day. i called my doc and they cut my dose and told me to cut salt. boom. 4 days later, back to normal. so simple. why do we make it so hard??
My feet are swollen. My doctor says it’s fine. I think I’m dying. I’m going to the ER. Now. I don’t care if it’s ‘just’ amlodipine. I’m not waiting.
Of course the article says ‘call your doctor’-but have you seen the wait times? My last appointment took 6 weeks. Meanwhile, my ankles look like overfilled water balloons. So I’ll just sit here, wait for my foot to fall off, and hope the system remembers I exist. Thanks for the reassurance, I guess.