Family-Based Treatment: What It Is and How It Helps with Mental Health and Addiction
When someone struggles with an eating disorder, addiction, or severe anxiety, family-based treatment, a structured therapy approach that includes family members as active participants in recovery. Also known as FBT, it’s not just about talking—it’s about rebuilding trust, reshaping habits, and creating a support system that lasts. Unlike traditional therapy that focuses only on the individual, this method recognizes that healing doesn’t happen in a vacuum. The people closest to you—parents, siblings, partners—play a real, measurable role in whether recovery sticks.
Family therapy, a broader category of counseling that addresses how relationships affect mental health is the umbrella under which family-based treatment falls. But FBT is more specific. It’s been proven effective for teens with anorexia, where parents take charge of meals until the child can manage it themselves. It’s used in opioid addiction recovery, where family members learn how to set boundaries without enabling. And it shows up in anxiety and depression treatment, where communication patterns that fuel stress are identified and changed together.
What makes this approach different? It’s action-driven. You don’t just discuss feelings—you practice new ways of speaking, eating, reacting, and responding. A parent might learn how to respond when their child refuses food. A spouse might learn how to stop covering up for their partner’s substance use. These aren’t abstract ideas—they’re daily skills practiced in real time.
Behavioral interventions, structured techniques designed to change harmful habits through repetition and reinforcement are the engine of family-based treatment. They’re not about blame. They’re about replacing old patterns with ones that support health. Studies show that when families are trained in these techniques, relapse rates drop significantly—especially in younger patients.
This isn’t just for teens or young adults. Adults with long-term addiction or mood disorders often benefit too. When a partner learns how to respond to panic attacks without panic, or when siblings stop enabling denial, the whole household shifts. Recovery becomes a shared mission, not a solo battle.
What you’ll find in the posts below are real stories and practical guides on how this approach works in practice. From how to handle medication side effects during recovery to how to avoid dangerous drug overlaps when multiple family members are on prescriptions, these articles connect the dots between mental health, physical health, and family dynamics. You’ll see how common meds like anticholinergics or benzodiazepines can complicate treatment, and how safe tapering strategies make a difference when the whole family is involved. Whether you’re a parent, caregiver, or someone in recovery, this collection gives you the tools to understand what’s really happening—and what to do next.
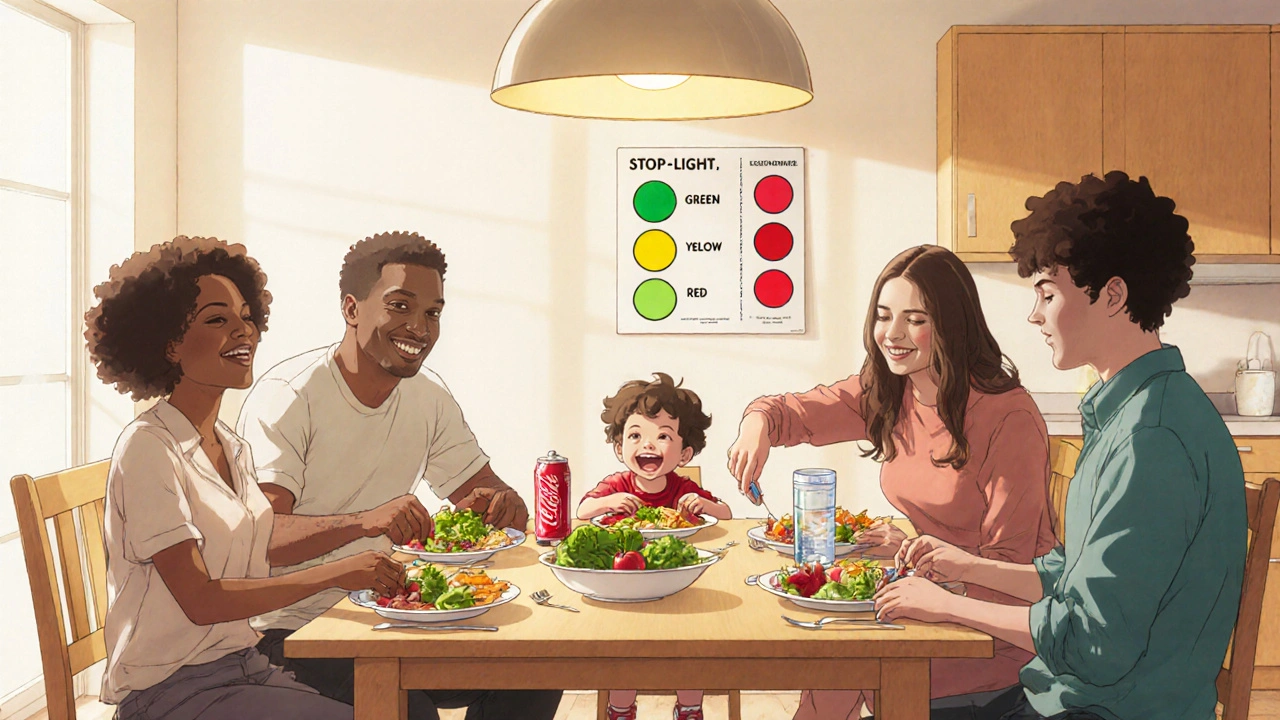
Childhood Obesity Prevention and Family-Based Treatment: What Works and Why
Childhood obesity affects 1 in 5 U.S. kids, but family-based treatment is the only proven method that works long-term. Learn how the Stoplight Diet, parent involvement, and daily habits can reverse the trend.