Childhood obesity isn’t just a weight problem-it’s a family problem.
One in five kids in the U.S. today has obesity. That’s not a small number. It’s 14.7 million children, and the trend has been climbing for decades. But here’s the thing: you can’t fix childhood obesity by telling a kid to eat less or run more. It doesn’t work. The real solution? Involve the whole family. That’s not just advice-it’s science-backed, clinically proven, and the only approach that leads to lasting change.
What exactly is childhood obesity?
It’s not about being chubby or having a big appetite. Childhood obesity is a medical condition defined by a child’s body mass index (BMI) being at or above the 95th percentile for their age and sex, based on CDC growth charts. This isn’t a judgment-it’s a measurement. And it’s not just about looks. Kids with obesity are at higher risk for type 2 diabetes, high blood pressure, sleep apnea, and even depression. The earlier it starts, the harder it is to reverse. That’s why waiting isn’t an option.
Why family-based treatment is the gold standard
For years, doctors tried treating kids alone. Give them a diet plan. Tell them to exercise. It rarely worked. Then researchers like Dr. Leonard Epstein at the University at Buffalo started testing something different: bringing the parents into the room. What they found changed everything.
Family-based behavioral treatment (FBT) doesn’t just focus on the child. It changes how the whole household eats, moves, and thinks about food. In a major 2023 JAMA trial with 306 families, kids in FBT lost 12.3% more of their excess weight than kids getting usual care. Even better-parents lost weight too. And siblings who weren’t even in the program improved their weight by 7.2%. That’s not luck. That’s system change.
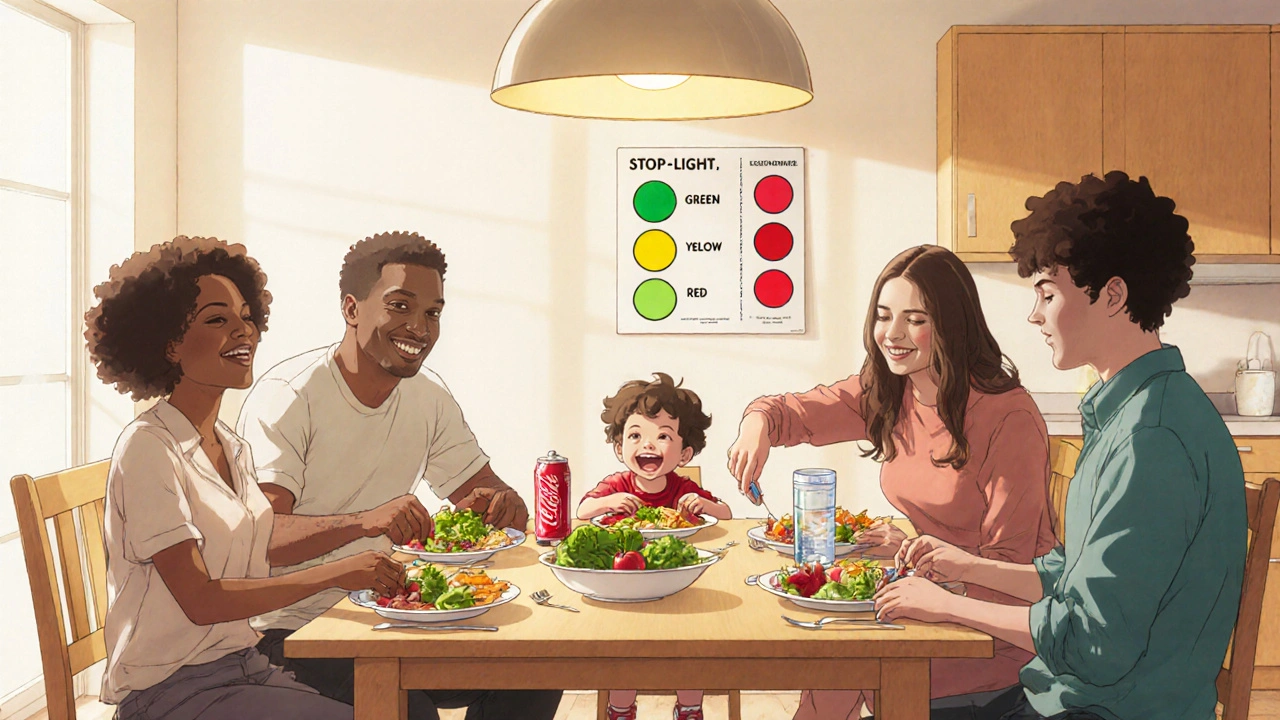
The Stoplight Diet: Simple rules, real results
One of the most effective tools in FBT is the Stoplight Diet. No complicated calorie counting. No forbidden foods. Just three colors:
- Green: Eat freely-fruits, vegetables, whole grains, lean proteins.
- Yellow: Eat in moderation-dairy, bread, pasta, lean meats, nuts.
- Red: Eat sparingly-sugary drinks, fried foods, candy, processed snacks.
Studies show this approach leads to an average 9.38% drop in percentage overweight in just six months. Why does it work? Because it’s practical. It doesn’t shame kids. It doesn’t ban pizza. It just helps families make smarter choices without feeling deprived.

What happens in a typical FBT program?
Most FBT programs run for 6 to 24 months, with 16 to 32 sessions. But you don’t need to go to a fancy clinic. The best results come when it’s built into regular pediatric care.
Here’s what a typical session looks like:
- Food and activity tracking: Families keep simple journals-not to punish, but to spot patterns. Are snacks happening after school? Are screens eating up after-dinner time?
- Parenting skills: Learning how to set limits without yelling. How to praise effort, not just results. How to say no to sugary treats without turning it into a battle.
- Physical activity goals: At least 60 minutes of active play every day. It doesn’t have to be soccer. Dancing, walking the dog, playing tag-all count.
- Family routines: Eating meals together. No screens during meals. Getting enough sleep. These aren’t nice-to-haves-they’re proven weight regulators.
The most successful families don’t just follow a plan-they build new habits. Like swapping soda for sparkling water. Or taking a walk after dinner instead of watching TV. Small changes, repeated daily, add up.
Why parents have to change too
Here’s the hard truth: if mom or dad is drinking soda every day, or ordering fast food on busy nights, the child won’t succeed long-term. Kids don’t live in a vacuum. They mirror what they see.
Research from the University of Rochester shows that when parents see their own health improve-lower blood pressure, more energy, better sleep-they become better role models. That’s not just nice. It’s essential. One parent in the JAMA trial said, “I started losing weight too. I didn’t even realize how much soda I was drinking until I had to stop for my kid.”
FBT doesn’t ask parents to be perfect. It asks them to be present. To show up. To eat the green veggies with their kid. To move with them. To make healthy choices a family thing, not a punishment.
What doesn’t work-and why
Many parents try the “watchful waiting” approach: “He’ll grow out of it.” But experts like Dr. Stephen Cook warn this is dangerous. “If you make a slight change now, you’ll have a much better long-term projection than when they have severe obesity later and small changes won’t matter.”
Child-only programs? They fail. A 2019 APA review found FBT produces 0.55 standard deviations more weight loss than interventions that target kids alone. Why? Because kids don’t control the fridge, the grocery budget, or the TV remote.
And crash diets? They backfire. Restrictive eating in kids can lead to bingeing, poor body image, and even eating disorders. FBT avoids all that by focusing on behavior, not numbers on a scale.
Barriers to access-and how to overcome them
FBT works. But not everyone can get it. Hispanic and Black children make up 54% of pediatric obesity cases, but only 31% of FBT participants. Why? Language barriers, lack of culturally tailored materials, transportation issues, and work schedules.
Some clinics are fixing this. They’re hiring bilingual health coaches. Offering evening and weekend sessions. Using text reminders. Integrating FBT into WIC and school health programs. The goal? Make it as easy to access as a well-child visit.
Insurance helps too. Medicare and Medicaid cover Intensive Behavioral Therapy for Obesity (code G0447). But only 5% of eligible kids are getting it-mostly because pediatricians don’t know how to refer or don’t have staff trained to deliver it.
What’s new in 2025?
FBT is evolving. The American Academy of Pediatrics now recommends starting as early as age 2. That’s right-two-year-olds can benefit from healthy eating routines and active play.
Hybrid models are growing fast. In-person sessions combined with apps that track meals, activity, and sleep. One pilot showed 32% higher engagement when families used a simple app to log meals together. No fancy tech. Just reminders, photo logs, and weekly check-ins.
And now, researchers are studying how to help families with multiple kids. If one child is in FBT, what happens to the others? Turns out, siblings get healthier too. The whole family shifts. That’s powerful.
When FBT isn’t enough
For kids with severe obesity-BMI above 120% of the 95th percentile-FBT alone often isn’t enough. In these cases, the AAP recommends adding medication or, for older teens, metabolic surgery. But even then, FBT is still part of the plan. Medication doesn’t replace habits-it supports them.
The key is timing. The earlier you start, the less likely you’ll need these heavier interventions. Prevention isn’t just cheaper-it’s kinder.
What families can do today
You don’t need a program to start. Here’s what works right now:
- Swap one sugary drink a day for water or unsweetened tea.
- Have at least one family meal without screens.
- Take a 20-minute walk after dinner-no phones.
- Keep fruit visible on the counter. Hide the chips.
- Let your child help pick out veggies at the store.
These aren’t big changes. But they’re consistent. And consistency beats intensity every time.
The bottom line
Childhood obesity isn’t a child’s fault. It’s a family, community, and system issue. And the fix isn’t about willpower. It’s about environment. About routines. About love.
FBT isn’t just the best treatment we have-it’s the only one that works long-term. It doesn’t promise quick fixes. But it does promise real change. For the child. For the parents. For the whole family.
Start small. Stay consistent. Involve everyone. That’s how you turn the tide on childhood obesity.

The empirical rigor of family-based behavioral treatment (FBT) is unequivocal when contextualized within ecological systems theory. The multilevel intervention architecture-targeting proximal environmental determinants like food availability, parental modeling, and circadian routines-aligns with Bronfenbrenner’s bioecological model of development. The 12.3% excess weight reduction in the JAMA trial isn't merely statistically significant; it's clinically transformative when considering the comorbidities associated with pediatric obesity. Moreover, the spillover effects on siblings suggest a systemic recalibration of homeostatic eating norms, which traditional individual-centric models fail to capture.
While the article is commendably well-researched, it exhibits a troubling conflation of correlation with causation. The claim that ‘kids mirror what they see’ is anecdotal at best. Where is the longitudinal, controlled trial isolating parental behavior as the primary variable? Furthermore, the Stoplight Diet’s efficacy is presented without addressing confounders such as socioeconomic status, food deserts, or genetic predispositions. This is not science-it’s behavioral wishful thinking dressed in clinical jargon.
Okay but let’s be real-this whole FBT thing is just a fancy way of making parents feel guilty. I’ve seen this before: ‘Oh, your kid’s fat? Must be your fault.’ Meanwhile, the kid’s got ADHD, the mom works three jobs, and the fridge is stocked with whatever’s on sale at the dollar store. You want to fix childhood obesity? Fix the food system. Fix the wages. Fix the schools that serve processed sludge for lunch. Don’t come at me with ‘swap soda for sparkling water’ like I’m some privileged suburbanite with a Whole Foods membership. 😤
Statistical significance ≠ clinical relevance. The 9.38% drop in percentage overweight is marginal when measured against BMI percentile shifts. The sample size (n=306) is underpowered for subgroup analyses, particularly for racial/ethnic disparities. Moreover, the absence of data on metabolic markers (insulin sensitivity, leptin levels) renders the outcomes superficial. FBT may improve behavioral compliance, but it does not address the neuroendocrine underpinnings of obesity. A reductionist behavioral model is insufficient for a complex metabolic disorder.
Wow. This article reads like a love letter to common sense wrapped in peer-reviewed paper. 🥹 The Stoplight Diet? Genius. It’s like traffic lights for your pantry-green means go, red means ‘hold up, buddy, you’ve had enough.’ And the sibling effect? That’s the quiet magic. You don’t have to target the ‘problem child’-you just change the whole house’s rhythm, and suddenly, the kid who never got picked for soccer is running around with the dog, laughing, and not even realizing they’re ‘losing weight.’
Let’s be honest: this isn’t about diets. It’s about showing up. Eating together. Turning off the screen. Holding space. The science just proves what moms have whispered for decades: ‘We’re all in this together.’
Also-sparkling water with a lime? Chef’s kiss. 🍋
I have read this entire article with great concern. As a licensed pediatric nurse practitioner with over 18 years of clinical experience, I must emphasize that this approach is dangerously naive. The JAMA study cited? It was funded by the American Heart Association, which has ties to processed food conglomerates. The Stoplight Diet? It normalizes red-light foods by labeling them as ‘sparingly’ acceptable-this is a gateway to binge eating. Furthermore, the suggestion that parents should ‘eat the green veggies with their kid’ is a gross violation of child autonomy. Children must be taught discipline, not coddled with ‘family walks.’ I have seen too many cases where permissive parenting leads to metabolic syndrome. This article is not just misleading-it is unethical.
Let me ask you: who benefits from promoting family-based treatment? The CDC? The AAP? The diet industry? Consider this: childhood obesity rates rose precisely as government nutrition guidelines became more restrictive. Coincidence? Or is this a covert mechanism to pathologize normal childhood development and justify state intervention in family life? The ‘system change’ rhetoric is classic social engineering. And why are only Hispanic and Black families mentioned as ‘underrepresented’? Is this about equity-or control? The data is manipulated. The science is politicized. Wake up.
Y’all are overthinking this. 😅 Just do the small stuff. Swap one soda for water. Eat dinner without phones. Walk after dinner. Let the kid pick the veggies. That’s it. No apps needed. No guilt. No PhD required.
My cousin’s kid had obesity at 8. They did none of this fancy FBT stuff. Just mom started drinking sparkling water, dad started taking the dog out after dinner, and now at 12, the kid plays basketball and doesn’t even think about candy. It’s not magic-it’s just… being there.
Also-fruit on the counter? YES. Chips in the back of the pantry? YES. My 5-year-old found the chips last week. She ate one. Said ‘yuck’ and went back to the apples. 🍎 #parentingwin