When you’re managing ADHD, the goal isn’t just to quiet the noise-it’s to build a life that works. For millions of people, that means finding the right mix of medication and strategies that actually fit into daily life. There’s no one-size-fits-all fix. What works for one person might leave another feeling drained, anxious, or just plain stuck. The truth is, ADHD treatment isn’t about picking one thing and calling it done. It’s about stacking tools-medication, habits, routines-that help you show up as your best self, day after day.
Stimulants: The Fast Track to Focus
Stimulants are the most common starting point for ADHD treatment, and for good reason. About 70 to 80% of people-kids and adults alike-see clear improvements in focus, impulse control, and task completion when they start taking them. These meds don’t make you hyper. They help your brain get out of the fog. Methylphenidate (like Ritalin or Concerta) and amphetamines (like Adderall or Vyvanse) work by boosting dopamine and norepinephrine in the prefrontal cortex-the part of your brain that handles planning, focus, and self-control.
Immediate-release versions kick in within 30 to 60 minutes and last about 3 to 4 hours. That means multiple doses a day, which can be tricky for school or work. Extended-release options like Concerta or Vyvanse last 10 to 12 hours, giving smoother coverage without the midday crash. Vyvanse is a prodrug, meaning it’s inactive until your body breaks it down-this makes it harder to misuse, which is why doctors often recommend it for teens or adults with a history of substance issues.
Side effects? They’re real. Appetite suppression hits 50 to 60% of users, especially kids. Sleep problems? Around 30 to 50% struggle to fall asleep. Headaches and stomachaches are common too. Some people report emotional blunting-feeling dull, flat, or less like themselves. On Reddit’s r/ADHD, nearly 70% of users say appetite loss never fully went away, and over half still battle sleep issues after years on medication.
Doctors usually start low: 5 mg of methylphenidate or 2.5 mg of amphetamine. Then they creep up by small amounts every week until symptoms improve or side effects become too much. It’s not a sprint-it’s a slow, careful tune-up.
Non-Stimulants: The Slower, Safer Path
If stimulants don’t work-or if side effects are too rough-non-stimulants are the next step. They’re not as fast, but they’re gentler on the body and carry no abuse risk. Atomoxetine (Strattera) is the most common. It works by increasing norepinephrine, which helps with focus and emotional regulation. But it takes 4 to 6 weeks to reach full effect. That’s a long time to wait when you’re struggling to get through the day.
Guanfacine (Intuniv) and clonidine (Kapvay) were originally blood pressure meds. Turns out, they also calm the overactive brain. They’re especially helpful for people with ADHD who also have tics, anxiety, or sleep issues. They don’t boost focus like stimulants, but they reduce impulsivity and emotional outbursts. Parents often report kids become less reactive and more patient after starting these.
Non-stimulants are less likely to cause appetite loss or insomnia. But they can cause drowsiness, dizziness, or low blood pressure-especially when you first start. They’re often used in combination with stimulants, not instead of them. For example, a child might take Vyvanse for focus during school and guanfacine at night to help with sleep and emotional control.
Cost matters too. Generic methylphenidate costs $15 to $25 a month. Brand-name extended-release stimulants? $250 to $400 without insurance. Strattera and Intuniv aren’t cheap either, but some insurance plans cover them better than stimulants. Step therapy rules-forcing you to try cheaper generics first-are common in the U.S. That can delay treatment by weeks.
Behavioral Strategies: Building Skills That Last
Medication helps you manage symptoms. Behavioral strategies help you build a life around them. Think of it like this: pills give you the energy to run. Strategies teach you how to run without tripping.
For kids, parent training is the gold standard. Programs like the New Forest Parenting Programme require 12 to 16 weekly sessions, each 90 minutes long. Parents learn to give clear, calm instructions, use reward systems instead of punishment, and stay consistent-even when it’s exhausting. Studies show this cuts parent-reported ADHD symptoms by 40 to 50%. It’s not magic. It’s muscle memory.
For adults, organizational tools make a huge difference. Digital calendars with reminders, task lists broken into tiny steps, timers for work blocks (Pomodoro technique), and designated “junk drawers” for clutter all help. One woman in Sydney told me she keeps a sticky note on her laptop that says: “What’s the next physical action?” That one question stops her from spiraling into overwhelm.
Schools matter too. Under the Americans with Disabilities Act (ADA) and similar laws in Australia, students with ADHD are entitled to accommodations: extra time on tests, quiet spaces, permission to move around, or even using a fidget tool. Teachers who understand ADHD don’t see a “bad kid.” They see a brain that needs different wiring.
Exercise isn’t just good for health-it’s a natural ADHD treatment. A 30-minute walk or bike ride before school or work can reduce impulsivity and improve focus for hours. It boosts dopamine the safe way.
What No One Tells You About Side Effects
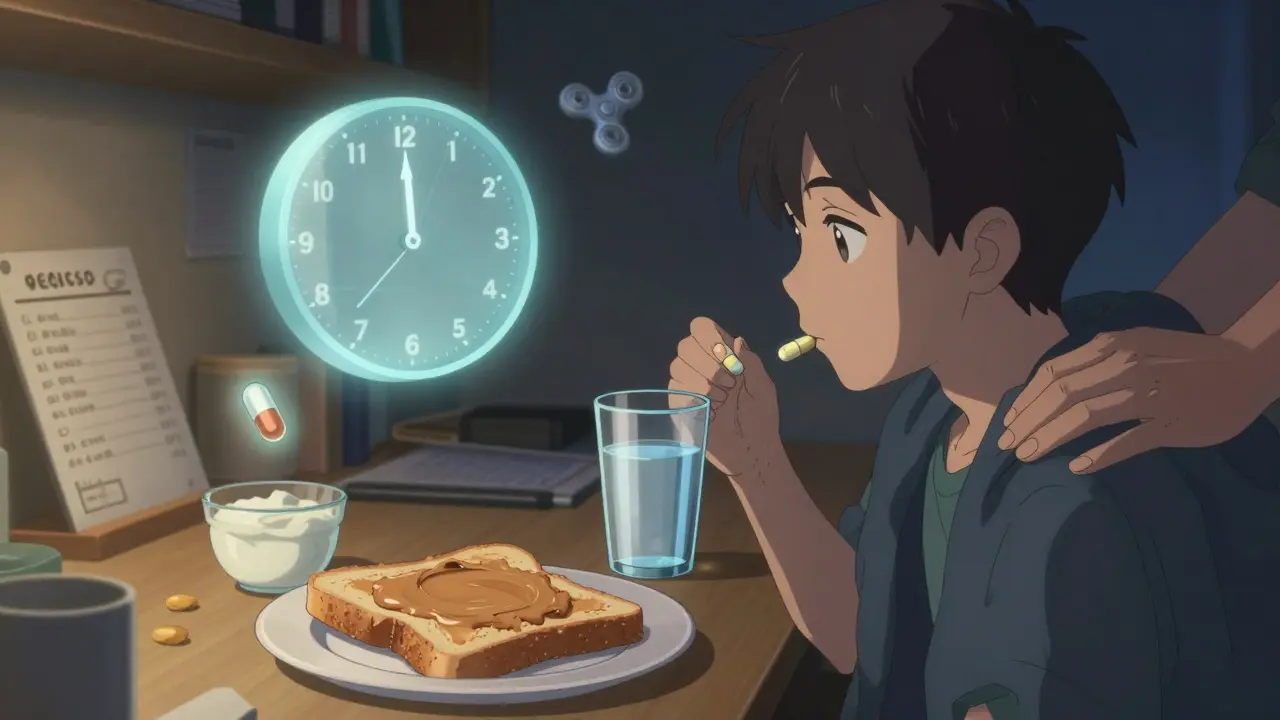
Side effects aren’t just annoying-they’re signals. Appetite loss? It often means the dose is working, but your body’s telling you it needs fuel. That’s why nutritionists recommend high-protein breakfasts before taking meds. A boiled egg, peanut butter on toast, or Greek yogurt can keep energy steady.
Sleep issues? Moving the last dose 6 to 8 hours before bedtime helps 65% of people. If you’re still struggling, try melatonin (3 mg, 30 minutes before bed). It’s not addictive, and studies show it helps with sleep onset in kids on stimulants.
Rebound effects-irritability or emotional crashes as the med wears off-are common in 45% of children. That’s not “bad behavior.” It’s neurochemistry. Timing a small, short-acting dose in the late afternoon can smooth the drop.
And growth? Yes, some kids slow down in height and weight the first year. But research shows it usually catches up by age 16. The American Academy of Pediatrics recommends checking height and weight every six months. If it’s dipping, talk to your doctor. It’s not a reason to quit meds-it’s a reason to adjust.
Gender, Age, and the Hidden Differences
ADHD doesn’t look the same for everyone. Girls and women are more likely to have inattentive-type ADHD, not hyperactivity. That means they’re often missed until adulthood. They’re the ones zoning out in class, not getting in trouble. Their meds might need lower doses because they report side effects 1.4 times more often than boys, according to studies from Qatar and Australia.
Preschoolers react differently too. Alpha-2 agonists like guanfacine cause less irritability and appetite loss in kids under 6 than stimulants. That’s why some pediatricians start there.
Adults with ADHD often have co-existing anxiety or depression. Stimulants can make anxiety worse. That’s why non-stimulants like atomoxetine or low-dose guanfacine are often better for adults with both ADHD and anxiety. And yes-some adults stop meds because they feel “numb.” That’s not a failure. It’s a sign to switch or adjust.

What’s New in 2026
The FDA approved AZSTARYS in 2023-a new combo drug that delivers dexmethylphenidate with a slow-release version to reduce misuse. It lasts 13 hours and has fewer peaks and crashes.
Screening for eating disorders before starting stimulants is now recommended. About 12% of people with ADHD have a predisposition to disordered eating, and stimulants can trigger it. If you or your child have a history of dieting, body image issues, or food restriction, tell your doctor.
Genetic testing is starting to enter the clinic. Tests like Genomind’s PGx Express look at your CYP2D6 and CYP2C19 genes to predict how you’ll metabolize stimulants. If you’re a slow metabolizer, you might need half the dose. If you’re a fast one, standard doses won’t work. It’s not perfect yet-but it’s getting closer to personalized ADHD care.
Digital therapies are here too. EndeavorRx, an FDA-cleared video game for kids 8 to 12, improves attention after 25 minutes of play, five days a week for four weeks. VR-based training programs are in phase 3 trials. They’re not replacements for meds-but they’re powerful partners.
When to Switch, Pause, or Stop
You don’t have to stay on meds forever. About 28% of kids in long-term studies stop by adolescence. Why? Side effects, feeling better, or just not wanting to be “the kid on pills.” That’s okay. Some people outgrow symptoms. Others learn coping skills that work better than pills.
But don’t quit cold turkey. Taper slowly under medical supervision. Stopping suddenly can cause fatigue, depression, or rebound ADHD symptoms that feel worse than before.
And if one med doesn’t work? Try another. Response varies wildly. One person might thrive on Vyvanse and hate Ritalin. Another might do the opposite. It’s not about willpower. It’s about biology.
There’s no shame in needing help. ADHD isn’t laziness. It’s a brain wiring difference. The right combination of meds and strategies doesn’t “fix” you-it lets you be who you are, without fighting your own brain every minute of the day.
Do stimulants make ADHD worse over time?
No. Long-term studies, including the 20-year follow-up of the MTA trial, show stimulants don’t harm adult outcomes. Some people develop tolerance, meaning they need higher doses, but that’s not the same as worsening ADHD. The real risk is untreated ADHD-academic failure, job loss, relationship strain, and higher rates of substance use. Medication reduces those risks.
Can you treat ADHD without medication?
Yes, but it’s harder. Behavioral therapy, exercise, sleep hygiene, and organizational tools can help, especially for mild cases. For moderate to severe ADHD, medication is far more effective. The MTA study found combination treatment (meds + behavioral therapy) worked better than either alone. If you’re avoiding meds, make sure you’re getting structured support-not just hoping things get better.
Why do some people say ADHD meds change their personality?
That usually means the dose is too high. When dopamine levels spike too much, people feel flat, quiet, or emotionally muted. It’s not who they are-it’s the medication overpowering their natural energy. Lowering the dose or switching to a slower-release version often fixes it. The goal isn’t to turn someone into a zombie. It’s to help them feel like themselves-just with less chaos.
Is it safe to take ADHD meds long-term?
For most people, yes. The FDA requires black box warnings for cardiovascular risks and abuse potential, but serious events are rare in healthy individuals. Regular check-ups-blood pressure, heart rate, height/weight-are key. If you have a history of heart disease, high blood pressure, or substance abuse, non-stimulants are safer. Always be honest with your doctor. There’s no such thing as too much info.
How do I know if my child’s ADHD meds are working?
Look for changes in daily life, not just grades. Can they start homework without a battle? Do they remember to bring their books home? Are they making friends without blurting out or interrupting? Teachers and parents should fill out behavior rating scales every 2 to 3 months. If the child is calmer, more organized, and less frustrated, the med is working-even if they’re still not perfect.
If you’re reading this because you or someone you love is struggling with ADHD, know this: you’re not broken. You’re just wired differently. The right tools-medication, routines, support-don’t erase ADHD. They let you live with it without letting it define you.



Been on Vyvanse for 5 years and honestly? It’s the only thing that lets me finish a sentence without my brain jumping to TikTok. Appetite’s trash, but I eat protein like it’s my job now. Also, walks before work? Game changer. I used to feel like a zombie by noon. Now I’m just a slightly tired human.
Also, why does everyone act like ADHD meds are magic? They’re not. They’re tools. Like a hammer. Doesn’t make you a carpenter, but it helps if you’re trying to build something.
Let me be clear: the notion that ADHD is a ‘brain wiring difference’-while poetically appealing-is a dangerously reductive anthropomorphization of neurochemistry. Dopamine dysregulation is not a ‘quirk,’ it is a neurobiological deviation with cascading executive dysfunction-yet society insists on romanticizing it as ‘creative energy.’
Medication is not ‘letting you be yourself’-it is pharmacologically overriding a pathological state. The goal is not ‘living with it’-it is restoring functional equilibrium. And yes, that means you might feel ‘numb’-because your brain was never meant to operate in perpetual overdrive.
omg i just found out my therapist is like 100% right abt non stimulants?? like i tried adderall and felt like a robot who forgot how to laugh?? then switched to strattera and now i can cry during dog videos again??
also why is everyone so obsessed with vyvanse? i got generic methylphenidate for $18 and it’s literally the same but i dont feel like i’m being microwaved from the inside.
ps: i spelled ‘meds’ wrong. sue me.
Reading this made me cry. Not because I’m sad-because I finally feel seen.
I’m 34, female, diagnosed at 30. I spent years thinking I was lazy. Turns out I just had a brain that needed structure, not shame. The sticky note thing? I stole that. Now I have one on my fridge: ‘What’s the next tiny thing?’
My kid’s on guanfacine. He used to scream when asked to put on socks. Now he says, ‘I need 2 minutes.’ That’s progress. Not perfection. Just progress.
And yeah, I still forget my keys. But now I know why. And that’s enough.
So let me get this straight-you’re telling me we’re supposed to believe some guy in a lab coat knows what’s best for my brain better than I do?
And you want me to take a pill so I can sit still while my boss micromanages me? No thanks. I’ll just keep being ‘unproductive’ and call it ‘anti-capitalist resistance.’
Also, why are all these studies funded by pharma? Coincidence? I think not.
Also also-why is everyone so obsessed with ‘focus’? What if I just want to zone out and watch clouds? Is that not a valid life choice?
Also also also-my dog doesn’t take meds. He’s fine.
Yo I just wanna say this article saved my life. I’ve been on and off meds for 8 years and I kept thinking I was failing because I couldn’t ‘just focus.’ But this? This is the first time someone explained that it’s not about willpower-it’s about chemistry.
Also, the part about growth in kids? My mom didn’t know that. She thought I was just being lazy. I lost 15 pounds in 6 months on Ritalin. She thought I was ‘on a diet.’
Now I tell people: ADHD meds aren’t a cure. They’re a bridge. And I’m still building mine.
Also-thanks for mentioning exercise. I started biking to work. I don’t need my 2nd dose anymore. My brain just… calms down. Like, naturally.
And yeah I typed ‘calms’ wrong. I’m tired. But I’m trying.
STOP acting like ADHD is just ‘a brain that needs different wiring.’ It’s not cute. It’s not quirky. It’s a disability that costs people jobs, relationships, and years of their life.
And if you think ‘behavioral strategies’ alone fix it-you’ve never tried to organize your life while your brain is screaming at you to check Instagram every 90 seconds.
Medication isn’t a crutch. It’s oxygen. And if you’re not taking it because you’re scared of being ‘numb’-you’re not brave. You’re just scared of being normal.
Also-yes, I’m aggressive. I’m tired of people romanticizing my suffering.
Dear fellow citizens of the modern neurodivergent dystopia,
One must question the hegemonic medical-industrial complex that pathologizes natural human variability under the guise of ‘treatment.’ The FDA’s approval of AZSTARYS is not progress-it is the commodification of attention. The genetic testing? A Trojan horse for corporate surveillance.
Consider this: if your child’s brain is ‘dysregulated,’ perhaps the environment is the pathology-not the child. Why not fix the school system? Why not reduce screen saturation? Why not allow children to move?
And yet-we are told to take pills. To conform. To be productive. The real ADHD, my friends, is the system that demands we be something we are not.
Yours in radical neurodiversity,
Sujit Paul, Ph.D. (in existential skepticism)
Look. I’m Canadian. We don’t do ‘stimulants.’ We do ‘warm tea and a hug.’
Also, why are all these studies American? Of course the data looks good-your healthcare system is a dumpster fire. You’re so desperate for a fix you’ll take a pill that makes your tongue feel like sandpaper.
And don’t get me started on ‘digital therapies.’ You’re letting kids play video games to treat ADHD? In Canada, we call that ‘weekend.’
Also, I once saw a man in a Vancouver park talk to his dog for 47 minutes. He was calm. Focused. Didn’t take a pill. Maybe the answer is not medicine-it’s more park time.
Just saying.
Let us not be naive. The pharmaceutical industry has weaponized neurodiversity as a market segment. The entire ADHD industrial complex is built on the exploitation of parental guilt, academic pressure, and the commodification of childhood. Genomind’s PGx test? A $1,200 placebo dressed in lab-coat rhetoric.
And yet-you, the reader, have been conditioned to believe that your child’s inability to sit still is a biochemical defect requiring corporate intervention. The truth? The system is broken. The pills are not the solution. They are the symptom.
What is the cost of ‘focus’ when it comes at the expense of emotional authenticity? When the child becomes a compliant cog? When the adult becomes a numb consumer of productivity?
We are not treating ADHD. We are erasing the very thing that makes us human.
-Aman Kumar, M.S. Neuroethics & Cultural Dystopia