Introduction to Cefixime: A Powerful Antibiotic
As a blogger who is always on the lookout for new and interesting topics to write about, I recently stumbled upon cefixime, a powerful antibiotic that has been proven to be effective in fighting bacterial infections. In this article, I will dive deep into the science behind cefixime to help you understand how it works and why it's such an important tool in our fight against bacteria. So let's begin our journey and explore the fascinating world of cefixime!
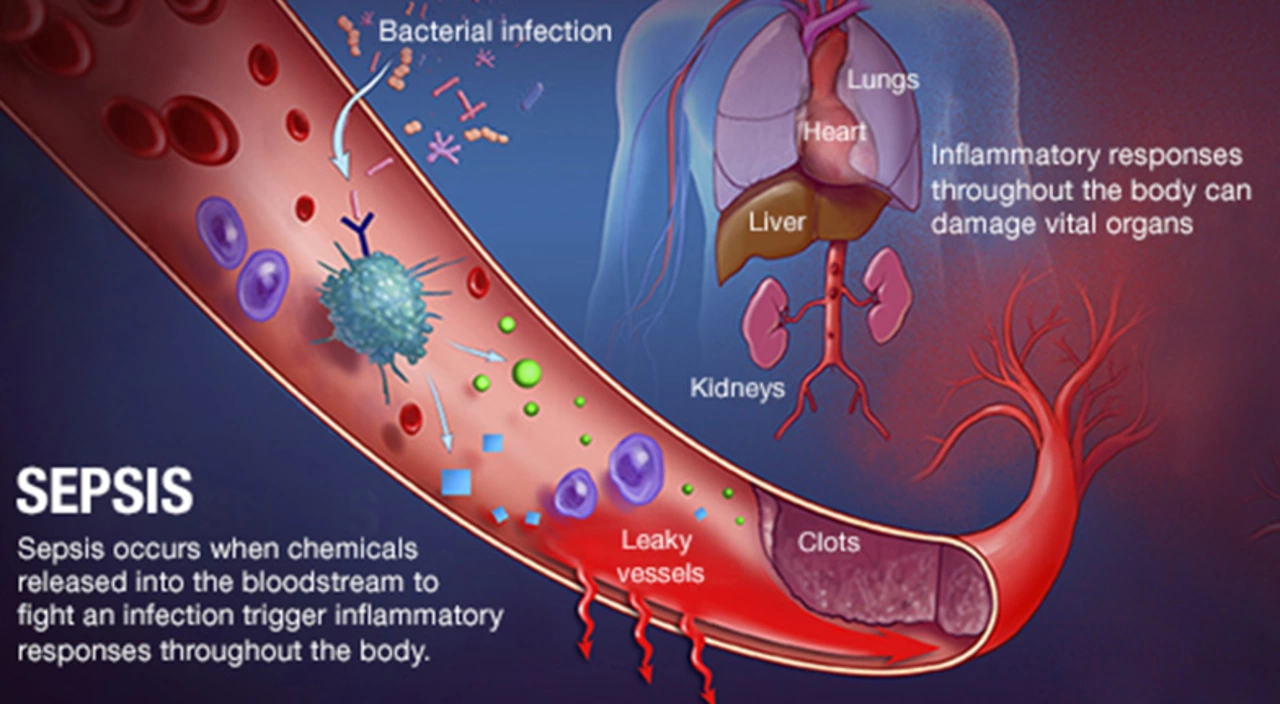
Understanding Bacterial Infections
Before we delve into the science behind cefixime, it's important to understand what bacterial infections are and how they can affect our bodies. Bacterial infections occur when harmful bacteria invade our body and start to multiply, causing an inflammatory response and potentially leading to a range of health problems. Some common examples of bacterial infections include strep throat, urinary tract infections, and pneumonia. In order to fight these infections, doctors often prescribe antibiotics, which are designed to kill or inhibit the growth of bacteria.
What is Cefixime?
Cefixime is a type of antibiotic known as a cephalosporin, which is part of a larger class of antibiotics called beta-lactams. These antibiotics are commonly prescribed to treat a wide variety of bacterial infections, including respiratory, urinary tract, and skin infections. Cefixime is particularly effective against Gram-negative bacteria, such as Escherichia coli and Klebsiella pneumoniae, which are responsible for many common infections.
The Science Behind Cefixime's Antibacterial Action
Now that we know what cefixime is and what it's used for, let's dive into the science behind how it works to fight bacterial infections. Like other beta-lactam antibiotics, cefixime works by targeting the bacterial cell wall. Bacteria have a unique cell wall structure that is critical for their survival and is not found in human cells. This makes the cell wall an ideal target for antibiotics like cefixime.
Inhibiting Cell Wall Synthesis
Cefixime works by inhibiting the synthesis of the bacterial cell wall, which is a complex structure made up of multiple layers. The key component of the bacterial cell wall is a substance called peptidoglycan, which provides strength and rigidity to the cell. Cefixime targets a specific enzyme called transpeptidase, which is responsible for cross-linking the peptidoglycan strands to form the cell wall. By inhibiting this enzyme, cefixime weakens the cell wall, leading to bacterial cell death.
Bactericidal vs. Bacteriostatic Effects
It's important to note that cefixime is considered a bactericidal antibiotic, meaning that it kills bacteria directly, rather than simply inhibiting their growth. This is in contrast to bacteriostatic antibiotics, which prevent bacteria from multiplying but do not directly kill them. Bactericidal antibiotics like cefixime are generally considered to have more potent antibacterial effects, making them a valuable tool in the fight against bacterial infections.
Resistance to Cefixime and the Importance of Proper Use
As with any antibiotic, it's crucial to use cefixime responsibly to minimize the risk of antibiotic resistance. Bacteria can develop resistance to antibiotics through various mechanisms, including the production of enzymes that break down the antibiotic, changes in the target enzyme or cell wall structure, or the development of efflux pumps that expel the antibiotic from the bacterial cell. These resistance mechanisms can be passed between bacteria through a process called horizontal gene transfer, allowing resistance to spread rapidly through bacterial populations.
Preventing Resistance Through Proper Use
To prevent the development of antibiotic resistance, it's important to use cefixime and other antibiotics responsibly. This means only using antibiotics when they are truly necessary and prescribed by a healthcare professional, taking the full course of antibiotics as prescribed, and not sharing antibiotics with others or using leftover antibiotics from a previous illness. By following these guidelines, we can help ensure that cefixime and other antibiotics remain effective tools in our fight against bacterial infections.
Side Effects and Interactions of Cefixime
Like all medications, cefixime can cause side effects and interact with other medications. Some common side effects of cefixime include gastrointestinal issues such as nausea, vomiting, and diarrhea, as well as headache and dizziness. It's important to inform your healthcare provider of any other medications you are taking, as cefixime may interact with them and cause adverse effects. For example, cefixime can enhance the effects of blood thinners, leading to an increased risk of bleeding.
Conclusion: The Power of Cefixime in Fighting Bacterial Infections
In conclusion, cefixime is a powerful antibiotic that works by targeting the bacterial cell wall, leading to the death of harmful bacteria. It is effective against a wide variety of bacterial infections, particularly those caused by Gram-negative bacteria. By understanding the science behind cefixime and using it responsibly, we can help ensure that it remains an effective tool in our fight against bacterial infections. So next time you or someone you know is prescribed cefixime, you can appreciate the fascinating science that makes this powerful antibiotic an important weapon in our battle against harmful bacteria.

Great overview of how cefixime works.
So you’ve finally decided to tackle the nitty‑gritty of a third‑generation cephalosporin – bravo!
Nothing says "fun Sunday read" like peptidoglycan cross‑linking, right?
But seriously, kudos for spelling out why we shouldn’t just hand out antibiotics like candy.
Understanding the mechanism helps us keep the good stuff effective for the people who actually need it.
I find it appalling that anyone would downplay the moral responsibility behind antibiotic use.
The article barely scratches the surface of the ethical consequences of overprescription.
People need to stop treating cefixime like a convenience and start thinking about future generations.
And btw the link to the study is broken – not helpful at all.
Enough said.
Hey, it’s good that you’re pointing out the responsibility – we all need that reminder 😊.
Cefixime is useful when doctors say you need it.
Take the full course and you’ll be okay.
I appreciate the enthusiasm, Laura, but it’s worth adding that not every infection warrants a cephalosporin.
Clinical guidelines often suggest narrow‑spectrum agents first.
Reserving cefixime for confirmed Gram‑negative cases helps curb resistance.
Let’s dive a little deeper into the pharmacodynamics and structural biochemistry of cefixime, because the surface‑level description, while helpful for lay readers, leaves out several critical nuances that are essential for both prescribers and microbiologists.
First, cefixime’s β‑lactam ring engages in a covalent acylation of the active‑site serine of penicillin‑binding proteins (PBPs), essentially creating a stable acyl‑enzyme complex that halts the transpeptidation step of peptidoglycan synthesis.
This inhibition is time‑dependent and exhibits what we term the post‑antibiotic effect (PAE), meaning that bacterial regrowth is suppressed even after plasma concentrations fall below the MIC.
Second, the molecule’s side‑chain – an aminothiazolyl moiety linked to a methoxyimino group – confers enhanced stability against many class A β‑lactamases, which is why cefixime retains activity against Enterobacteriaceae that produce TEM‑1 or SHV‑1 enzymes.
However, it remains vulnerable to extended‑spectrum β‑lactamases (ESBLs) and AmpC-type enzymes, so susceptibility testing is non‑negotiable before empirical therapy in high‑risk settings.
Third, the drug’s renal excretion pathway (approximately 85% unchanged in urine) necessitates dose adjustments in patients with creatinine clearance <30 mL/min, as accumulation can precipitate neurotoxic manifestations such as encephalopathy or seizures.
Fourth, resistance mechanisms beyond β‑lactamase production include alterations in PBP affinity – for instance, the acquisition of PBP‑3 mutations in *Neisseria gonorrhoeae* has been linked to reduced cefixime susceptibility, prompting public‑health authorities to revise treatment guidelines.
Fifth, the pharmacokinetic profile-bioavailability of about 50% with a half‑life of 3–4 hours-means that standard dosing (400 mg once daily) achieves peak serum concentrations sufficient to exceed the mutant prevention concentration (MPC) for most target pathogens, thereby limiting the selection of resistant subpopulations.
Sixth, clinicians should be wary of drug–drug interactions; cefixime can potentiate the anticoagulant effect of warfarin via displacement from plasma proteins, increasing INR values and bleeding risk 📈.
Seventh, in terms of adverse event spectrum, while gastrointestinal upset is most common, rare cases of severe Clostridioides difficile infection have been documented, underscoring the need for antimicrobial stewardship programs to monitor usage trends.
Eighth, from a public‑health perspective, judicious prescribing of cefixime contributes to preserving the efficacy of the entire cephalosporin class, which remains a cornerstone in the treatment of multidrug‑resistant Gram‑negative infections.
Finally, education of patients about the importance of completing the full therapeutic course cannot be overstated; premature discontinuation is a primary driver of emerging resistance patterns worldwide.
In summary, cefixime’s mechanism is a classic example of β‑lactam inhibition of cell‑wall synthesis, enhanced by structural features that confer β‑lactamase stability, but its optimal use demands careful consideration of pharmacokinetics, resistance mechanisms, and patient‑specific factors. 😊