Unraveling the Mystery: Helicobacter pylori's Role in Stomach Ulcers
There's no denying that our bodies are magical, complex entities that can sometimes feel like they're utterly confounding. The mystery of how a tiny single-celled organism, the Helicobacter pylori, can wreak havoc on our digestive tract and contribute to stomach ulcers is one such enigma that has left even the brightest minds scratching their heads. But worry no more! By the end of this article, you'll not only know how this tiny organism can cause so much discomfort but also be armed with tips on how to tackle it.
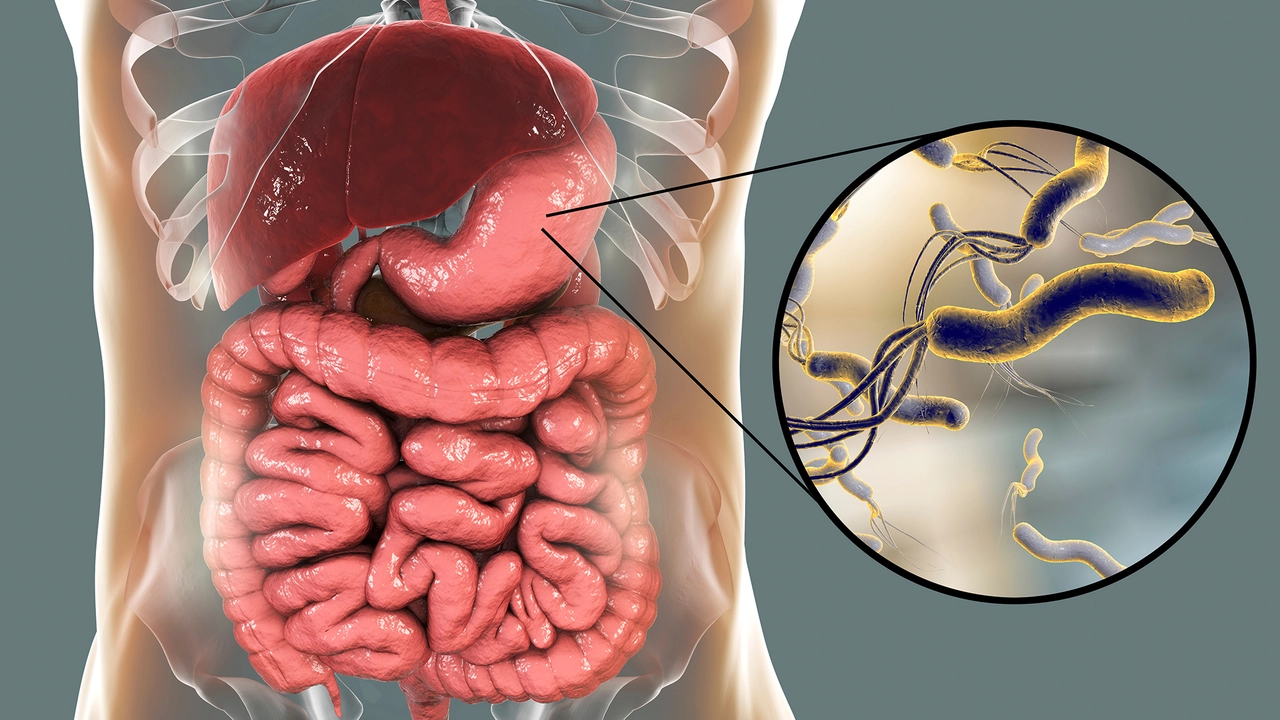
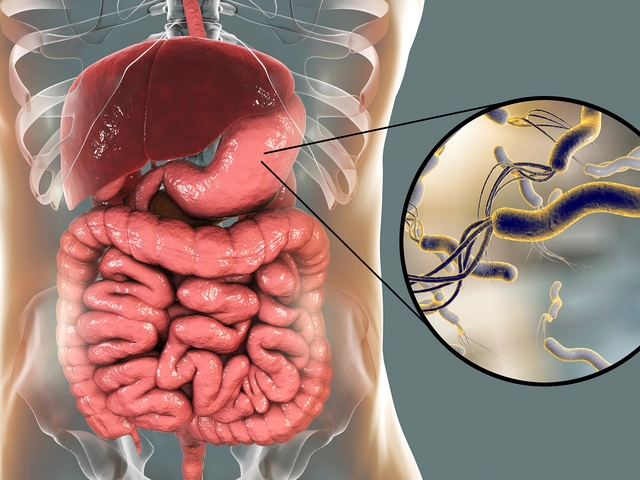
The Invader: Meet Helicobacter pylori
Before we dive deep into the mystical realm of our gut, let's get introduced to the alleged culprit - Helicobacter pylori. You've perhaps never seen this microbe before, unless you have been hard at work in a lab with a high-powered microscope. This bacterium, tiny enough to make a grain of sand seem like a vast desert, takes up residence in your stomach and unfortunately does more than just help you digest your food.
One peculiar fact I find quite amusing about H. pylori is how it fares in one of the harshest environments known to man - our stomach. I mean, our stomachs dissolve food into a pulpy semi-fluid mass using strong acids, imagine living in that! Let's say by some sheer misfortune, a comet smashes into planet Earth and evaporates all water, creating a world not unlike our stomach environment – strong acid rains, sizzling heat – but somehow, this cheeky little bacterium would probably still survive. Quite the little hardcore survivalist, isn't it?
The Crime: Stomach Ulcers and their Experimental Culprit
Now, onto the crime scene. Stomach ulcers, also known as gastric ulcers, are sores that form on your stomach lining. Contrary to the widely accepted belief, it's not always that spicy vindaloo or late-night pizza that causes stomach ulcers (although they certainly can trigger it). These painful sores can commonly trace their roots back to H. pylori. But, how does this tiny, seemingly harmless organism cause such discomfort?
Well, it seems our uninvited guest, H. pylori, besides just surviving in the acid rain of our stomach, has another trick up its sleeve. Just like that pen you misplaced but find behind your ear or that toy car Lawson "misplaces" in my shoes every now and then (not cool, Lawson, not cool), H. pylori has its sneaky ways. It produces a substance that neutralizes stomach acid, allowing it to stealthily colonize the stomach lining and, in the process, triggers some unwelcome irritation that could lead to ulcers.
Unfolding the Plot: The Connection Between H. pylori and Stomach Ulcers
So, here's where things get a tad bit more complex. Now, it's important to note that not everyone infected with H. pylori develops ulcers - sort of like how not all Australians get to own a kangaroo, even though we are surrounded by them. As it turns out, whether you develop ulcers or not depends on factors like your genetics, environmental factors, and other health conditions. It's like the ultimate annoying lottery, which you definitely don't want to win.
No matter how the specifics play out, though, the end result is the same-- a breach in the protective lining of the stomach or small intestine. It makes the perfect 'playground' for H. pylori, turning our stomach into its very own amusement park. But in contrast to the fun and frolic of an amusement park, this usually involves a lot of pain, bloating, nausea, and other discomforts that have you hugging the toilet bowl at odd hours.
The Intervention: Preventing Stomach Ulcers Caused by H. pylori
Now, it might seem like all hope is lost. A tiny invader wreaking havoc in your body, seemingly unstoppable, like Phoebe when she's got a hold of my lipstick (believe me, the bathroom mirror didn't see it coming). But, thankfully, when it comes to H. pylori and stomach ulcers, we've got more ammunition at our disposal than a damp washcloth.
There are medications available that can help eradicate H. pylori from our bodies, sort of like how a properly conducted clean-up drive can remove almost any trace of Phoebe's lipstick disaster from the bathroom walls. Medications such as proton pump inhibitors and antibiotics normally do the trick. But, let's not forget - preventive measures are always better than cures, much like securely hiding my makeup is far more effective than spending hours scrubbing walls.
Closing the Case: The Verdict on H. pylori and Stomach Ulcers
While H. pylori might be one of the common culprits behind stomach ulcers, it's crucial to remember that there are other causes too, like excessive use of certain painkillers and alcohol. Just remember, like everything else in life, moderation and balance are key. And a healthy conversation with your doctor will never go astray.
In the end, remember that we’re all on this crazy roller-coaster ride of life, equipped with a body that's nothing short of a wonderland. Even when things go awry and unwelcome guests like H. pylori try to crash the party, remember – we have the capacity, knowledge, and humor to bounce back, and maybe learn some intriguing facts along the way! So here's to discovering more about ourselves, keeping it light, and making life a little less perplexing one fact at a time!

Got this, you can beat H. pylori with the right regimen. Stick to the prescribed antibiotics, add a proton pump inhibitor, and give your gut some time to heal. Consistency is key, so don’t skip doses.
I totally get how unsettling this info can be. The good news is that most doctors have a clear protocol for eradication, and side effects are usually manageable. Just keep an eye on your symptoms and stay in touch with your physician. It’s also helpful to avoid NSAIDs while you’re healing. Remember, you’re not alone in this.
Honestly, the whole H. pylori hype is overblown. Many people live with the bacteria and never develop ulcers, so the panic is unnecessary. Focus on lifestyle factors instead of blaming a microbe for everything.
One must consider that the pharmaceutical industry has a vested interest in promoting antibiotic regimens for H. pylori. The data presented often downplays natural immunity and the role of diet. It is plausible that undisclosed side‑effects are being concealed deliberately. Moreover, the narrative conveniently aligns with profit‑driven motives, raising legitimate concerns about bias.
Helicobacter pylori remains one of the most extensively studied gastric pathogens, and its association with peptic ulcer disease is supported by a substantial body of epidemiological evidence. The organism’s urease activity enables it to neutralize gastric acid, creating a microenvironment conducive to colonization of the mucosal layer. Once established, H. pylori expresses cytotoxins such as CagA and VacA, which disrupt epithelial integrity and provoke inflammatory responses. Chronic inflammation leads to mucosal atrophy, impaired mucus production, and ultimately ulcer formation. Numerous randomized controlled trials have demonstrated that eradication therapy, typically comprising a proton pump inhibitor, clarithromycin, and amoxicillin or metronidazole, markedly reduces ulcer recurrence rates. Furthermore, systematic reviews indicate that successful eradication lowers the incidence of gastric cancer by up to 40 % in high‑risk populations. The mechanisms underlying these benefits involve restoration of normal gastric pH, reduction of pro‑inflammatory cytokines, and re‑establishment of a balanced microbiota. Adherence to the full therapeutic course is essential, as incomplete treatment can foster antimicrobial resistance. Resistance patterns vary geographically; therefore, susceptibility testing is advisable when first‑line therapy fails. In addition to pharmacologic measures, lifestyle modifications such as limiting NSAID use, reducing alcohol consumption, and avoiding smoking complement medical treatment. Dietary interventions rich in antioxidants and probiotics may further support mucosal healing, though evidence remains preliminary. It is also noteworthy that not all colonized individuals develop pathology; host genetic factors, bacterial virulence, and environmental exposures synergistically influence disease manifestation. Consequently, a personalized approach that integrates clinical, microbiological, and lifestyle assessments yields the most favorable outcomes. Ongoing research continues to explore vaccine candidates and novel agents aimed at minimizing the public health burden of H. pylori‑related disease.
The article glosses over the profound implications of antibiotic resistance arising from blanket H. pylori treatment. By presenting eradication as a panacea, it neglects the long‑term ecological impact on the gut microbiome. This omission is not merely an oversight; it reflects a dangerous bias toward pharmaceutical solutions.
I appreciate the balanced view that combines medical therapy with lifestyle advice. It’s reassuring to see that the author acknowledges both pharmacologic and non‑pharmacologic strategies.
Sure, because we all love a good cocktail of antibiotics and PPIs-nothing says “fun” like a side‑effect profile that reads like a horror novel.
People should stop ignoring the moral responsibility of diet.
You’re right! 🌟 Keep the positivity flowing and remember that with the right plan, you’ll beat this.