Treatment-Resistant Depression: What Works When Standard Treatments Fail
When someone has treatment-resistant depression, a form of major depressive disorder that doesn’t improve after at least two different antidepressant trials at adequate doses and durations. Also known as refractory depression, it affects about 1 in 3 people who seek help for depression—meaning it’s not rare, it’s just often misunderstood. This isn’t about being "weak" or "not trying hard enough." It’s a biological reality: your brain’s chemistry isn’t responding the way it should to standard drugs like SSRIs or SNRIs, even when taken exactly as prescribed.
What makes it resistant? Sometimes it’s genetics. Other times, it’s coexisting conditions like anxiety, thyroid problems, or chronic pain that mask or worsen the depression. Some people have inflammation in their brain, or their stress response system is stuck in overdrive. That’s why simply switching from one antidepressant to another often doesn’t help. You need a different approach entirely. That’s where TMS, transcranial magnetic stimulation—a non-invasive procedure that uses magnetic pulses to stimulate nerve cells in the mood-regulating parts of the brain comes in. Or electroconvulsive therapy, a well-studied, highly effective treatment that triggers a brief seizure under anesthesia to reset brain activity. These aren’t last-resort options anymore—they’re proven tools, backed by data, and used daily in clinics worldwide.
And it’s not just about drugs or devices. Therapy matters—especially CBT and DBT—but when depression is this deep, talk therapy alone rarely moves the needle. That’s why the best outcomes happen when you combine treatments: maybe TMS plus a new antidepressant, or ECT followed by ongoing counseling. Even lifestyle changes like sleep hygiene, light exposure, and movement play a role. But here’s the thing: if you’ve tried three or four meds and still feel stuck, you’re not broken. You just haven’t found the right combination yet.
The posts below cover real-world strategies that help people break through this wall. You’ll find guides on how to avoid dangerous drug overlaps when juggling multiple prescriptions, what to ask your doctor when standard meds fail, and how certain medications—like anticholinergics or benzodiazepines—can accidentally make depression worse. There’s also practical advice on managing side effects, recognizing when a treatment is working (or not), and how to navigate the system when insurance and access become barriers. This isn’t theoretical. These are stories from people who’ve been where you are—and found a way forward.
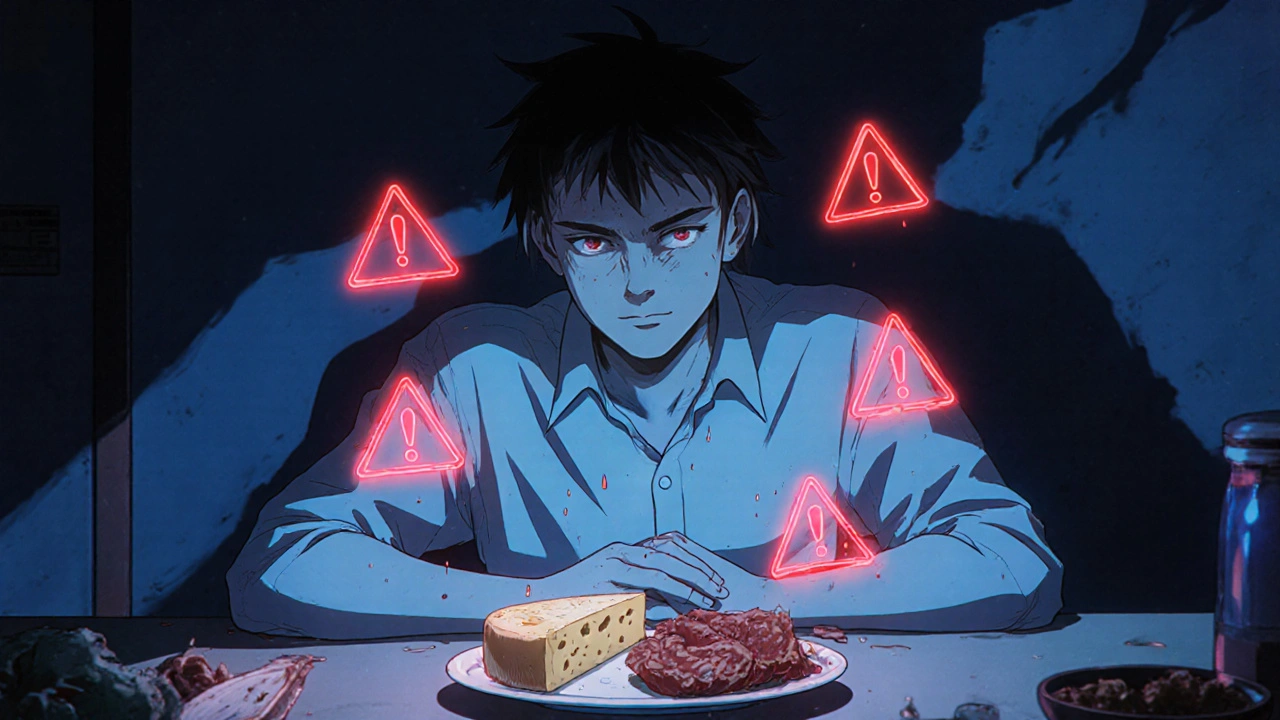
Monoamine Oxidase Inhibitors: What You Need to Know About Side Effects and Dietary Restrictions
MAOIs are powerful antidepressants for treatment-resistant depression, but they come with strict dietary rules and dangerous drug interactions. Learn how they work, what to avoid, and who they're really for.