Duplicate Medications: Avoid Double Dosing and Dangerous Overlaps
When you’re taking more than one pill for the same condition, you might not realize you’re doubling your dose—that’s what duplicate medications, when two or more drugs with the same active ingredient are taken together, often unknowingly. Also known as medication duplication, it’s a silent risk that affects thousands, especially older adults and people managing multiple chronic conditions. You could be taking amoxicillin for an infection and then pick up a generic version under a different brand name, not knowing they’re the same thing. Or maybe you’re on sildenafil for erectile dysfunction and add another pill with the same active ingredient because it’s marketed as "stronger" or "faster." These aren’t just mistakes—they’re preventable health emergencies.
Drug interactions, how one medication affects another in your body. Also known as pharmacological interactions, it is the real danger behind duplicate meds. Take anticholinergics like Benadryl and oxybutynin together? You’re stacking side effects—dry mouth, confusion, memory loss. Combine multiple QT-prolonging drugs? You risk Torsades de Pointes, a life-threatening heart rhythm. Even something as simple as taking two different statins like Zocor and another cholesterol pill can spike muscle damage risks. These aren’t hypotheticals—they show up in real patient stories, like those who ended up in the ER after mixing generic and brand-name versions of the same drug.
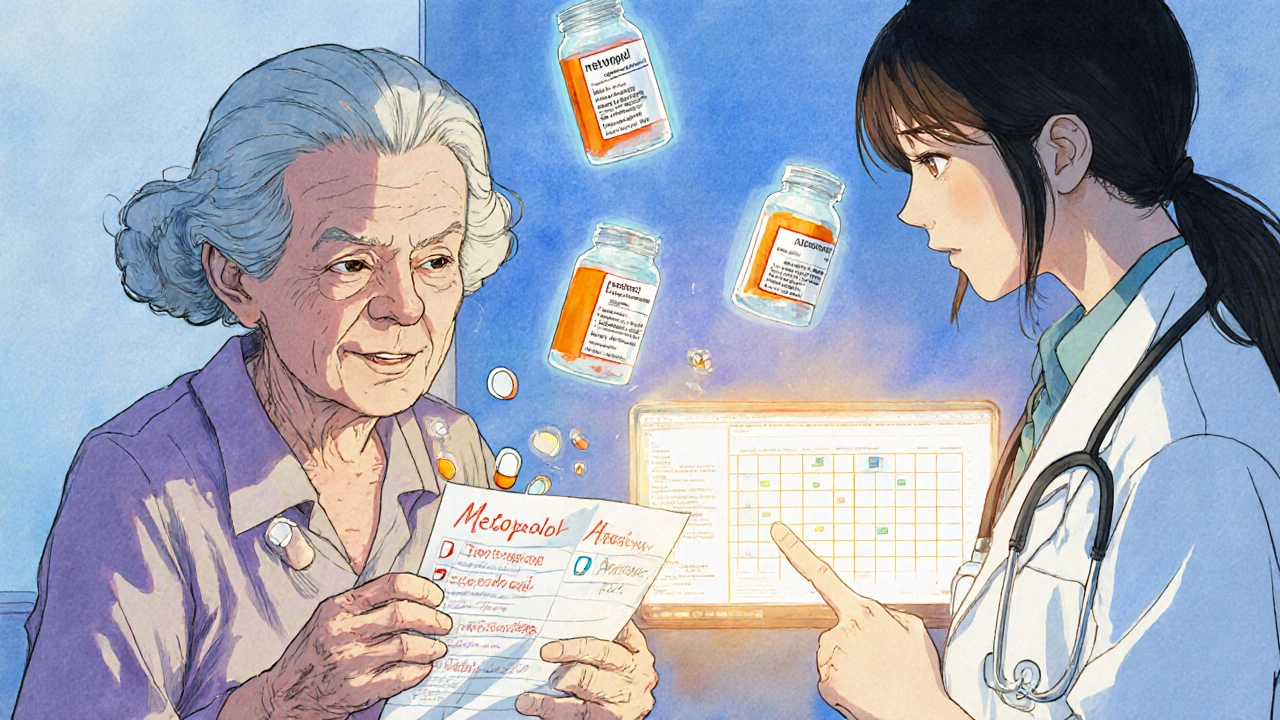
Polypharmacy, the use of multiple medications at once, often five or more. Also known as multiple drug therapy, it isn’t always bad—sometimes it’s necessary. But when it’s poorly managed, it becomes a breeding ground for duplicates. A patient might get a new prescription from a specialist without telling their primary doctor, or refill a leftover antibiotic from last year while starting a new one. This is why checking your full list with your pharmacist isn’t optional—it’s essential. You don’t need to remember every name or dose. Just bring all your bottles, pills, and supplements to one appointment. Let someone else see the full picture.
And it’s not just about pills. Some supplements and OTC meds hide active ingredients you’re already taking. Zinc oxide and benzalkonium chloride? They’re in dandruff shampoos, but if you’re also using a topical acne treatment with the same compounds, you’re overloading your skin. Acarbose and metformin? Both help with blood sugar, but using them together without guidance can cause low blood sugar or GI distress. Even something as common as Tylenol and cold medicine can sneak in extra acetaminophen—enough to damage your liver.
What you’ll find below isn’t just a list of articles. It’s a practical toolkit. You’ll see real comparisons between similar drugs—like how Cenmox stacks up against Augmentin, or how P-Force Fort compares to Cialis. You’ll learn how to spot hidden duplicates in everyday meds, understand why some drugs are prescribed together (and why others shouldn’t be), and get clear, no-fluff advice on how to talk to your doctor or pharmacist before you take another pill. This isn’t about fear. It’s about control. You have the right to know exactly what’s in your body—and why.
How to Avoid Duplicate Medications After Specialist Visits
Learn how seniors can avoid dangerous duplicate medications after specialist visits by keeping a full medication list, using one pharmacy, asking the right questions, and working with their primary care doctor to prevent harmful drug overlaps.