Graves' disease is the most common cause of hyperthyroidism in the United States, affecting about 1 in 200 people. It’s not just an overactive thyroid-it’s your immune system mistakenly attacking your own thyroid gland. This triggers the production of abnormal antibodies that force the thyroid to pump out too much hormone, throwing your whole body out of balance. If left untreated, it can lead to heart problems, bone loss, or even a life-threatening crisis called thyroid storm. But there are treatments-and one of them, propylthiouracil (PTU), plays a critical role, especially for certain patients.
What Happens When Your Immune System Attacks Your Thyroid
Your thyroid is a small butterfly-shaped gland at the base of your neck. It controls your metabolism-how fast you burn energy, how your heart beats, even your mood. In Graves’ disease, your immune system creates something called thyroid-stimulating immunoglobulin (TSI). These antibodies act like fake keys, slipping into the thyroid’s receptors and telling it to produce more hormones than your body needs.
The result? High levels of free T4 and T3, and a suppressed TSH (thyroid-stimulating hormone) below 0.4 mIU/L. Common symptoms include rapid heartbeat, unexplained weight loss, shaky hands, trouble sleeping, and intense anxiety. About 78% of patients report severe anxiety and insomnia before diagnosis, often leading to misdiagnosis as panic disorder or menopause.
Graves’ disease doesn’t just affect your thyroid. In 25-50% of cases, it causes eye problems-bulging eyes, redness, double vision. This is called Graves’ ophthalmopathy. In 1-4% of cases, it causes thick, red skin on the shins or feet, known as dermopathy. These signs help doctors distinguish Graves’ from other causes of hyperthyroidism.
Why PTU Is Still Used Despite the Risks
There are three main treatments for Graves’ disease: antithyroid drugs, radioactive iodine, and surgery. Antithyroid drugs like methimazole and propylthiouracil (PTU) are usually the first step. They block your thyroid from making too much hormone. Methimazole is preferred for most adults because it’s taken once a day and has fewer serious side effects.
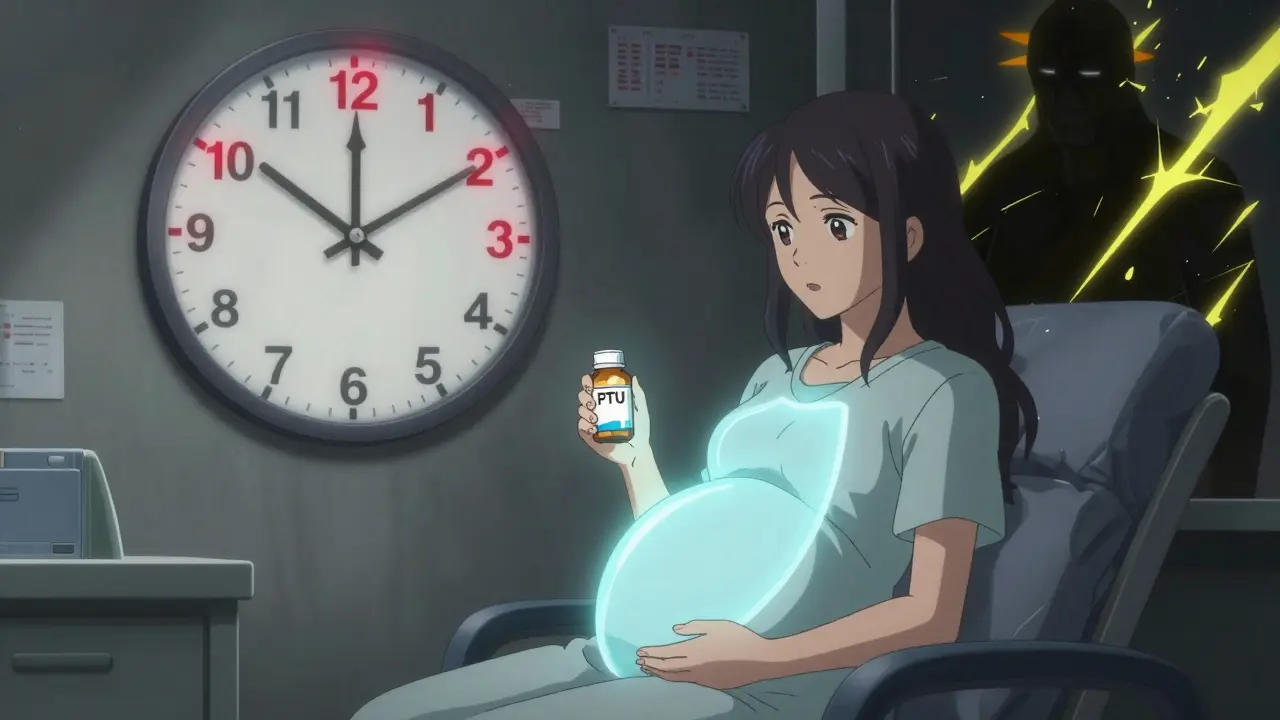
But PTU has one unique advantage: it’s safer in early pregnancy. Methimazole can cause birth defects if taken in the first trimester. PTU crosses the placenta less and carries a lower risk of fetal harm. That’s why doctors choose PTU for pregnant women in the first 12 weeks. The American Thyroid Association still recommends it for this group, even though PTU carries a higher risk of liver damage.
Severe liver injury from PTU happens in 0.2-0.5% of patients. It’s rare, but dangerous. Symptoms include jaundice (yellow skin), dark urine, nausea, or right-sided abdominal pain. That’s why anyone on PTU needs monthly liver function tests. One patient shared on a health forum: “PTU saved my pregnancy, but the constant liver checks were stressful-I had ALT levels spike to 120 U/L (normal <40) at week 24.”
Other side effects of PTU include taste changes (reported by 32% of users), joint pain (18%), and rare but serious drops in white blood cells (agranulocytosis). If you develop a fever or sore throat while on PTU, stop taking it and call your doctor immediately.
How PTU Compares to Other Treatments
Let’s look at how PTU stacks up against the other options.
| Treatment | How It Works | Pros | Cons | Cost (USD) |
|---|---|---|---|---|
| PTU (Propylthiouracil) | Blocks thyroid hormone production | Safe in early pregnancy; fast-acting in thyroid storm | Higher liver toxicity risk; needs 3x daily dosing | $10-$30/month |
| Methimazole | Blocks thyroid hormone production | Once-daily dosing; lower liver risk | Higher risk of birth defects in first trimester | $10-$50/month |
| Radioactive Iodine (I-131) | Destroys overactive thyroid cells | Permanent cure; single dose | Leads to lifelong hypothyroidism; not for pregnant women | $300-$1,500 |
| Thyroidectomy | Surgical removal of thyroid | Immediate results; no radiation | Surgical risks: nerve damage, low calcium | $5,000-$15,000 |
Radioactive iodine is the most common long-term solution in the U.S., curing hyperthyroidism in 80-90% of cases. But nearly all patients end up needing daily thyroid hormone replacement for life. Surgery is fast and definitive, but it’s invasive. PTU and methimazole are temporary fixes-they don’t cure the disease, they just control it.
After 12-18 months of antithyroid drug therapy, about 30-50% of patients go into remission. But 40-60% relapse within a year of stopping the medication. That’s why doctors often recommend long-term monitoring even after symptoms disappear.
Who Needs PTU-and Who Should Avoid It
PTU isn’t for everyone. It’s reserved for:
- Pregnant women in the first trimester
- Patients with thyroid storm (a medical emergency)
- People who can’t tolerate methimazole due to side effects
It’s not recommended for:
- Non-pregnant adults (methimazole is safer)
- People with pre-existing liver disease
- Those who can’t commit to monthly blood tests
Doctors now use a blood test called TRAb (thyrotropin receptor antibody) to predict relapse. If levels stay above 10 IU/L after treatment, there’s an 80% chance the disease will come back. This helps decide whether to keep using drugs or move to radioactive iodine.
What Life Looks Like on PTU
Starting PTU means adjusting to a new routine. You’ll need to take it three times a day, usually with meals. Missing a dose can cause hormone levels to spike again. You’ll also need regular blood work-every 4-6 weeks at first, then every 2-3 months once stable.
Many patients feel better within 2-3 months. Heart rate slows, anxiety eases, weight stabilizes. But eye symptoms often linger. About 40% of people still have bulging eyes or dryness even after their thyroid levels are normal. For these cases, newer treatments like teprotumumab (a targeted injection) can reduce eye swelling by 71%, though it costs over $150,000 per course.
Smoking makes eye complications worse. If you smoke and have Graves’ disease, quitting is one of the most important things you can do.

When to Call Your Doctor
While on PTU, watch for these warning signs:
- Yellow skin or eyes (sign of liver damage)
- Fever or sore throat (possible agranulocytosis)
- Severe nausea or abdominal pain
- Heart rate over 100 bpm at rest
- Temperature above 100.4°F (could signal thyroid storm)
Thyroid storm is rare but deadly-mortality rates are 20-30% if not treated immediately. It usually happens when Graves’ disease is untreated or poorly controlled, often triggered by infection, surgery, or trauma.
Looking Ahead: What’s New in Graves’ Treatment
The treatment landscape is changing. In 2021, the FDA approved teprotumumab for Graves’ eye disease-the first drug specifically designed for it. Clinical trials are now testing TSH receptor blockers and B-cell therapies like rituximab, which showed 60% remission in tough cases.
A new home monitoring device called ThyroidTrack, approved in 2022, lets patients check their TSH levels at home with lab-grade accuracy. It’s not widely available yet, but it could one day reduce the need for frequent clinic visits.
Researchers are also studying genetic markers like HLA-DR3, which increases Graves’ risk threefold. In the future, treatment may be tailored based on your genes, not just your symptoms.
For now, PTU remains a lifeline-for pregnant women, for those in thyroid storm, and for others who have no other options. It’s not perfect, but it’s necessary. And for many, it’s the difference between chaos and control.
Is PTU safe during pregnancy?
Yes, PTU is the preferred antithyroid drug during the first trimester of pregnancy because it carries a lower risk of birth defects compared to methimazole. After the first 12 weeks, doctors often switch patients to methimazole to reduce the risk of liver damage. Regular liver function tests are required throughout pregnancy.
Can Graves’ disease be cured?
Antithyroid drugs like PTU and methimazole don’t cure Graves’ disease-they control it. About 30-50% of patients go into remission after 12-18 months of treatment. But relapse rates are high-40-60% within a year of stopping medication. Radioactive iodine and surgery can permanently stop thyroid overactivity, but they lead to lifelong hypothyroidism, requiring daily hormone replacement.
Why is PTU used for thyroid storm?
Thyroid storm is a life-threatening emergency caused by extremely high thyroid hormone levels. PTU works faster than methimazole because it also blocks the conversion of T4 to the more active T3 hormone in the body. This dual action makes it the preferred drug in emergencies, even though it carries higher risks in routine use.
What are the long-term side effects of PTU?
The most serious long-term risk is liver damage, which can be sudden and severe. Other side effects include joint pain, taste changes, and low white blood cell counts. These risks are why PTU is not used long-term unless absolutely necessary. Monthly blood tests are mandatory to catch problems early.
Do I need to avoid certain foods or supplements with PTU?
Yes. Avoid large amounts of iodine-rich foods like seaweed, kelp, and iodized salt, since iodine can make hyperthyroidism worse. Also avoid supplements containing iodine, such as some multivitamins and cough syrups. Always check labels or ask your pharmacist.
Next Steps: What to Do If You’re Diagnosed
If you’ve been diagnosed with Graves’ disease, start by finding an endocrinologist who specializes in thyroid disorders. Use the American Thyroid Association’s provider directory to locate one near you. Ask about TRAb testing to understand your relapse risk. If you’re pregnant, discuss PTU versus methimazole timing with your doctor and obstetrician.
Keep a symptom journal: track your heart rate, weight, sleep, and mood. This helps your doctor adjust your dose faster. Join a support group-many patients say talking to others who’ve been through it makes a huge difference.
And if you’re on PTU: never skip your blood tests. Liver damage doesn’t always cause obvious symptoms until it’s too late. Your monthly blood work isn’t just a formality-it’s your safety net.



Bro, I was diagnosed with Graves’ last year and PTU was my first shot. Felt like my body was on fire one day, then suddenly I’m taking a pill that makes me feel like a zombie. Liver tests every week? Yeah, that’s not a hobby, that’s a second job.
But hey, at least I didn’t lose my eyesight. My coworker had the bulging eyeballs thing-looked like he was permanently shocked by a toaster. Weird as hell, but real.
And yeah, PTU’s a beast, but if you’re preggo and you don’t want your kid to come out looking like a science experiment, you take it. No debate.
I still remember the day I Googled ‘anxiety + weight loss + heart racing’ and it spat back ‘Graves’ disease.’ I cried. Not because I was scared-but because for the first time, someone had a name for the chaos inside me.
PTU? I took it for 8 months. My skin turned yellowish. Not dramatic, but enough to make me stare in the mirror like ‘is this me or a horror movie prop?’
They switched me to methimazole. Felt like a betrayal. Like my body said ‘you’re not special enough for the risky one.’
Still, I’m alive. Still, I’m here. And I still hate that my immune system is a traitor.
PTU is a pharmaceutical trap. Big Pharma knows it causes liver failure so they push it on pregnant women because they’re vulnerable. They want you to think it’s safe because it’s ‘the only option’-but what if the real option is just not being poisoned in the first place?
Have you ever heard of selenium? Or iodine restriction? No? That’s because they don’t make money off it. The thyroid is a puppet. And they’re pulling the strings.
They’ll give you a pill. Then another pill. Then a biopsy. Then a scan. Then a surgery. All to keep you hooked. Wake up.
It’s critical to contextualize the risk-benefit calculus of PTU versus methimazole in gestational hyperthyroidism. The relative risk of hepatotoxicity with PTU is approximately 0.3% in the first trimester, whereas methimazole carries a 1-3% risk of embryopathy, particularly aplasia cutis and choanal atresia.
Moreover, placental transfer kinetics demonstrate that PTU’s protein binding reduces fetal exposure by 40-60% compared to methimazole, which is freely diffusible. The ATA guidelines are not arbitrary-they’re evidence-based, grounded in longitudinal cohort studies from the 1990s onward.
Dismissing pharmacotherapy as ‘toxic’ without understanding pharmacokinetics is not just irresponsible-it’s dangerous pseudoscience.
Why do we even let foreigners tell us what’s safe? In America, we’ve got the best doctors, the best labs, the best science. But now we’re told to trust some pill made in a lab overseas just because it’s ‘safer for babies’?
My cousin took PTU and ended up in the ICU. Liver failure. They didn’t even test her properly. This isn’t medicine-it’s Russian roulette with a prescription.
And don’t get me started on how they push this on pregnant women like it’s a goddamn vitamin. We’re not lab rats. We’re Americans.
You think your body is broken? It’s not. It’s trying to tell you something. Graves’ isn’t a disease-it’s a signal. Your body’s screaming for balance. You’re not failing because you need a pill. You’re failing because you’re ignoring the truth.
PTU? That’s just another band-aid on a bullet wound.
Try fasting. Try grounding. Try removing gluten. Try sleeping under a copper wire. Your thyroid isn’t broken-it’s betrayed. And you’re giving it poison instead of peace.
I healed mine with breathwork and a salt lamp. No drugs. No scans. No fear. You can too. Stop letting them sell you sickness.
I read the whole thing. Twice. Then I looked up the original 1948 study on PTU. Funny thing-it was developed by a German chemist who fled the Nazis. He didn’t care about profits. He cared about saving lives.
Now we’ve got people calling it a conspiracy. That’s not skepticism. That’s forgetting history.
Also, the liver toxicity? Yeah, it’s real. But so is thyroid storm. One kills fast. The other kills slow. You pick your poison.
And if you’re pregnant? You don’t get to be a hero. You get to be a parent.
Minor grammatical error in the original post: ‘ALT levels spike to 120 U/L (normal’ is an incomplete sentence. Should be ‘normal range is 7–56 U/L’ or similar. Also, ‘thyroid-stimulating immunoglobulin (TSI)’ should be capitalized consistently. And ‘mIU/L’ needs a space before the unit. Small things, but they matter.
Also, PTU’s half-life is 1.5–2 hours. That’s why it’s dosed TID. Methimazole is 12–24 hours. That’s the real reason for the dosing difference-not safety. Just saying.
For anyone on PTU: if your ALT goes above 100, talk to your endo immediately. I had a spike at 130-scared the crap out of me. But we caught it early, switched meds, and I’m now in remission after 3 years.
Don’t panic. Don’t quit cold turkey. But don’t ignore the numbers. Your liver isn’t just a organ-it’s your body’s filter. Treat it like the MVP it is.
And if you’re pregnant? You’re not alone. I was too. PTU saved my daughter’s life. I’ll never regret it.
Everyone’s acting like PTU is the villain. But what if the real villain is the system that forces people into a binary: poison or panic?
Why can’t we have better drugs? Why are we stuck with 70-year-old chemistry because the market’s too lazy to invest? Why is pregnancy the only time we ‘make exceptions’ for toxicity?
Graves’ isn’t a medical mystery. It’s a societal failure. We treat symptoms, not causes. We medicate, not heal. We fear the pill, but never the system that made the pill necessary in the first place.
So yeah-PTU’s dangerous. But so is pretending we’ve fixed anything.