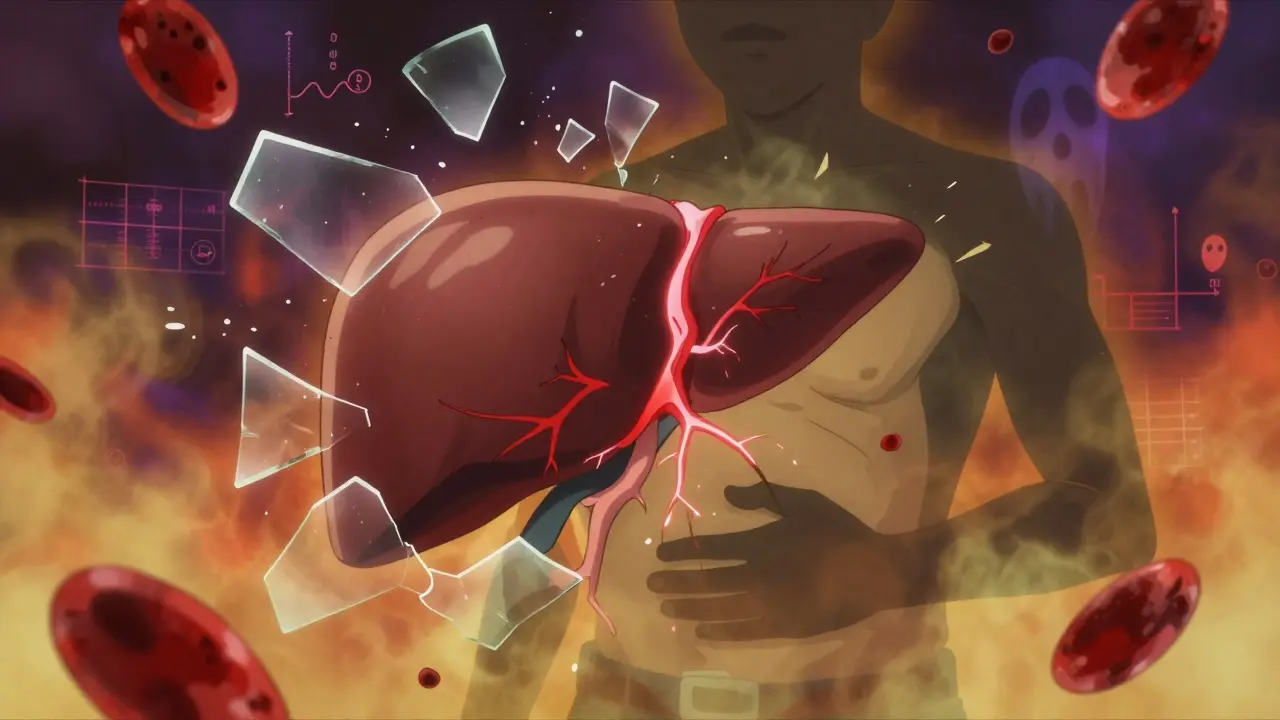
Most people don’t realize their liver is silently breaking down until it’s too late. Alcohol-related liver damage doesn’t come with a warning siren. It creeps in quietly, often without symptoms, until one day you’re jaundiced, swollen, or struggling to think clearly. By then, the damage may already be severe. But here’s the truth: alcoholic liver disease isn’t a single event-it’s a progression, and each stage offers a chance to stop it.
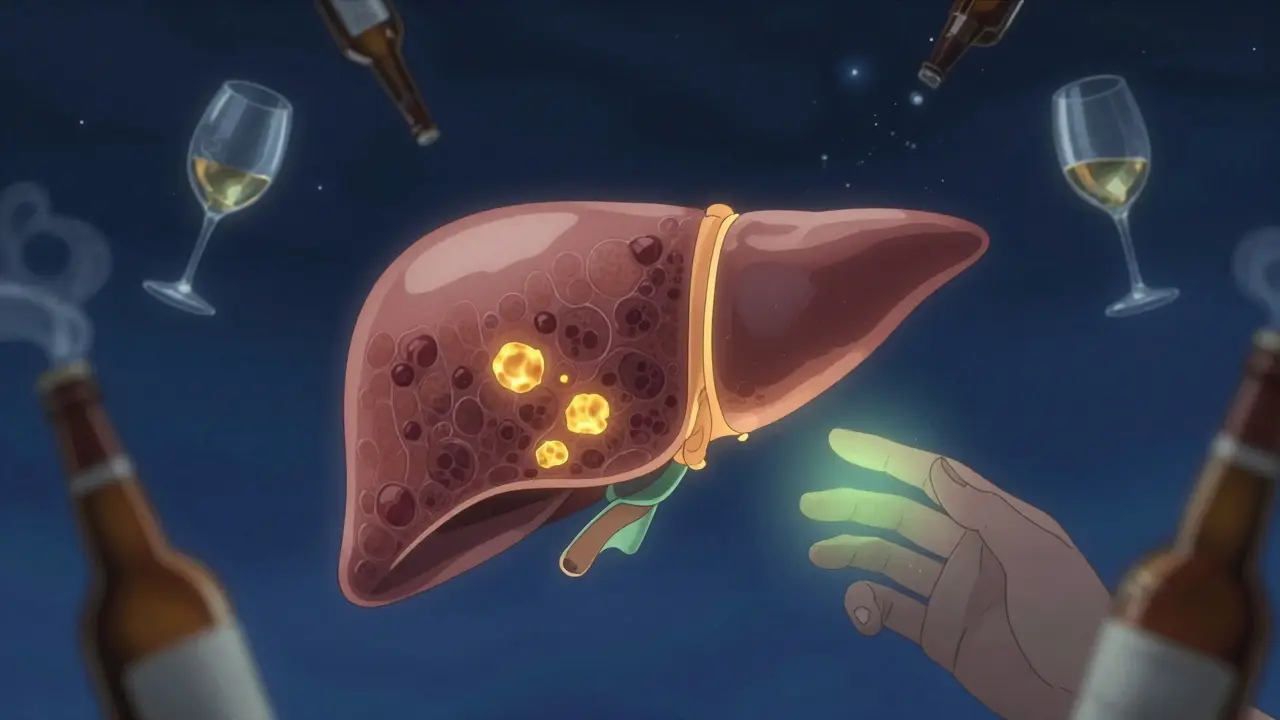
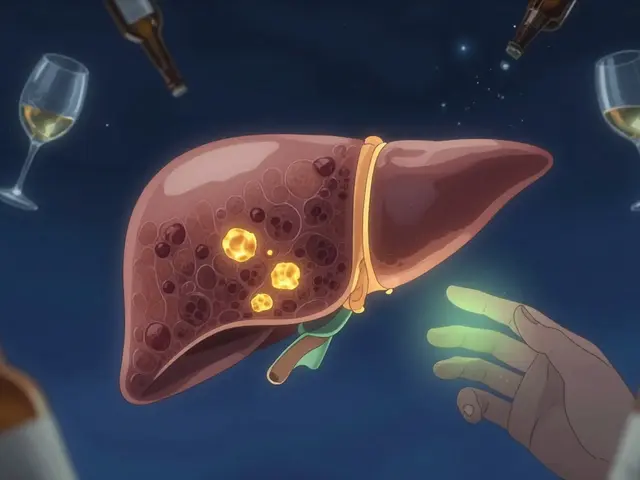
Stage 1: Fatty Liver (Alcoholic Steatosis)
This is where it starts-for 90% of people who drink heavily, fat builds up in the liver within days. You might have had a few too many weekend drinks, or maybe you’ve been having two glasses of wine every night for years. Either way, your liver is storing excess fat because it’s overwhelmed trying to process alcohol.
At this point, you probably feel fine. No pain. No yellow skin. No bloating. That’s why it’s so dangerous. Blood tests might show slightly elevated liver enzymes-AST and ALT-but even those can be normal. The only real sign? A scan showing fat covering more than 5-10% of your liver weight.
The good news? This stage is completely reversible. If you stop drinking for just 4 to 6 weeks, your liver clears out the fat. In one clinical trial, 85% of people saw their liver return to normal after quitting alcohol. No meds. No surgery. Just abstinence. It’s the most effective treatment you’ll ever get for liver disease.
Stage 2: Alcoholic Hepatitis (Alcohol-Associated Hepatitis)
If you keep drinking, the fat doesn’t just stay there-it turns into inflammation. This is alcoholic hepatitis, or what doctors now call alcohol-associated hepatitis (AH). Around 30-35% of people with fatty liver develop this if they keep drinking over several years-or sometimes after a single binge of 100 grams of alcohol (about 8 standard drinks) in one day.
Symptoms start showing now. Yellow eyes and skin (jaundice). Belly swelling from fluid buildup (ascites). Fever. Nausea. Confusion. Fatigue so deep it feels like your bones are made of lead. These aren’t just "feeling off" signs-they’re red flags.
Doctors use a test called the Maddrey Discriminant Function (mDF) to measure severity. If your score is above 32, you’re in severe AH. Without treatment, 30-40% of people with severe AH die within a month. Even mild cases carry a 4-10% risk of death in 30 days.
Treatment? First, stop drinking-immediately. Then, steroids like prednisolone may be given for severe cases. The STOPAH trial showed steroids lowered 28-day death rates from 20% to 18%. That might not sound like much, but in liver disease, even a 2% drop saves lives. And for those who respond, the liver can heal-partially or fully-if alcohol is gone.
But here’s the catch: nearly half of people with severe alcoholic hepatitis have never been told they had liver problems before. The disease hides in plain sight.
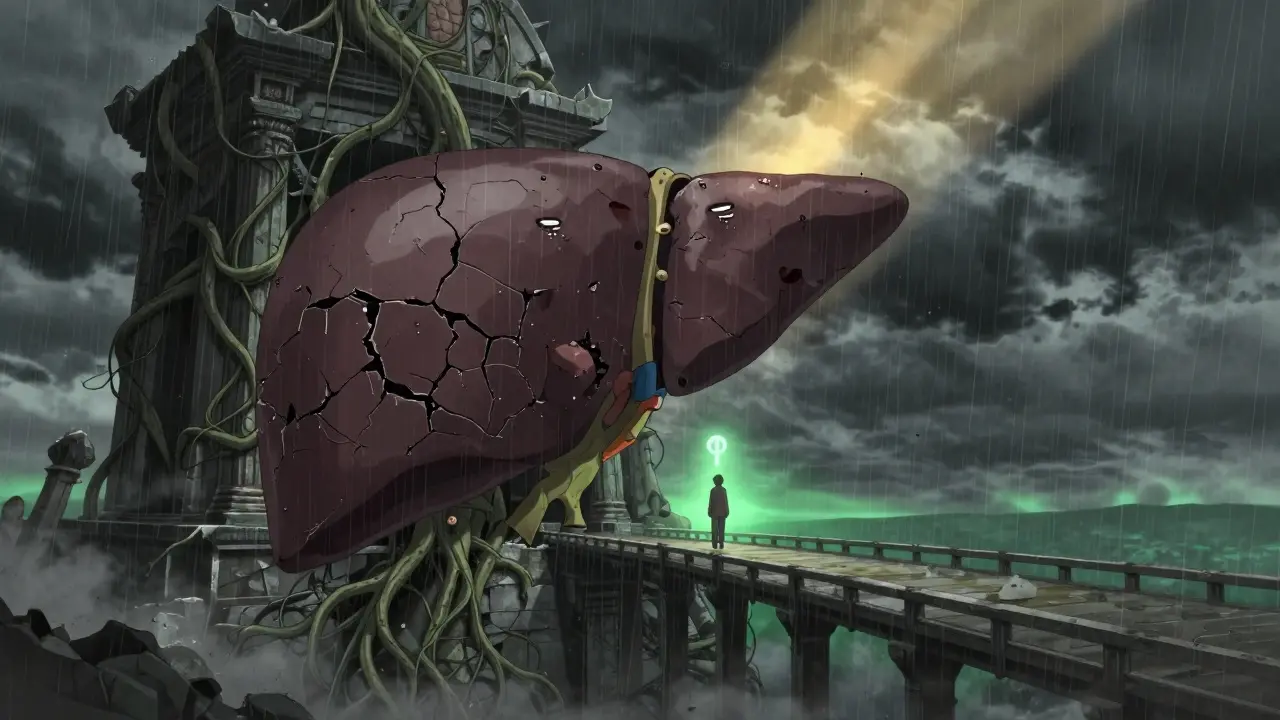
Stage 3: Cirrhosis (Alcohol-Associated Cirrhosis)
Cirrhosis is the point of no return-or so people think. It’s when scar tissue replaces healthy liver cells. More than 75% of the liver’s normal structure is gone. The organ can’t filter toxins, make proteins, or store energy like it used to.
About 10-20% of heavy drinkers reach this stage. It takes years-usually 10 or more-of consistent drinking. But women develop it faster, often after less alcohol, because their bodies process it differently.
At this stage, symptoms get worse. Swelling in the legs and belly. Vomiting blood from burst veins in the esophagus. Mental confusion (hepatic encephalopathy). Kidney failure. Weight loss. Skin itching. These aren’t side effects-they’re signs your liver is failing.
Here’s what most don’t know: cirrhosis isn’t always a death sentence. If you stop drinking completely, 50-60% of people with early-stage cirrhosis stabilize. Their liver stops getting worse. Their survival rate jumps from 30% to 70-90% over five years. Abstinence is the single most powerful intervention at this stage.
But if you keep drinking? Median survival drops to just 1.8 years. The liver keeps scarring. Complications pile up. Transplant becomes the only option.
Liver transplants work-70-75% of patients survive five years after surgery. But most centers won’t list you unless you’ve been sober for at least six months. That’s not punishment. It’s survival math. People who relapse after transplant have a 70% chance of dying within two years.
What Makes It Worse?
Not everyone who drinks heavily gets liver disease. Why? Genetics, gender, and other health issues play a huge role.
Women are 2-3 times more likely to develop damage at lower alcohol levels. People with certain gene variants-like PNPLA3 or TM6SF2-have a higher risk. If you also have obesity, diabetes, or hepatitis C, your liver is under double or triple stress. Even moderate drinking (20-40 grams a day) can speed up scarring if you already have fatty liver from other causes.
And here’s something rarely talked about: stigma. Many people delay seeing a doctor because they’re ashamed. One survey found 45% of patients felt judged by healthcare workers instead of helped. That delays diagnosis by years. By the time they get in, it’s often too late.
How Is It Diagnosed?
Doctors don’t wait for symptoms. They look for patterns. Heavy drinking history? Check. Elevated AST and ALT? Check. AST higher than ALT? That’s a classic sign. An ultrasound might show fat. A FibroScan (a painless ultrasound-based test) can detect scarring without a biopsy.
Liver biopsy used to be the gold standard. Now, non-invasive tools like FibroScan and blood tests like the ALive panel (in late-stage trials) can spot early fibrosis with over 85% accuracy. These tools are changing everything-catching damage before it’s irreversible.
What Can You Do?
There’s no magic pill. No supplement that fixes this. Only one thing works: stopping alcohol.
If you’re in stage one-fatty liver-quit now. Your liver will thank you in weeks.
If you’re in stage two-alcoholic hepatitis-quit immediately. Get medical help. Steroids might help. But only if you stop drinking.
If you’re in stage three-cirrhosis-quit anyway. It’s not about reversing damage. It’s about surviving. Stopping alcohol can double or triple your life expectancy.
Support matters. People who get help from both liver specialists and addiction counselors have a 65% chance of staying sober after one year. Those who go it alone? Only 35% make it.
There are new treatments on the horizon-gut microbiome transplants, anti-inflammatory drugs, targeted therapies. But none of them work without sobriety.
Who’s at Risk Right Now?
It’s not just middle-aged men anymore. Hospitalizations for alcoholic liver disease have jumped 65% among 25-34-year-olds since 2010. Women in this group are seeing the steepest rise. Why? Social drinking has normalized. Binge drinking is common. And no one tells you your liver doesn’t bounce back forever.
Lower-income communities are hit hardest. Rates are more than three times higher than in wealthier areas. Access to care? Limited. Stigma? Heavy. Prevention? Rare.
This isn’t just a "drinker’s problem." It’s a public health crisis hiding in plain sight.
Real Stories
One man, 38, found out he had fatty liver after a routine blood test. He cut out alcohol. Six months later, his liver enzymes were normal. He’s now a fitness coach.
A woman, 47, kept drinking after her doctor warned her about elevated enzymes. She ended up in the hospital with jaundice and ascites. She survived. But she’s now on the transplant list. She says: "I thought I had control. I didn’t."
Another, 52, stopped drinking after his third hospitalization for alcoholic hepatitis. He’s been sober for five years. His liver still has scars, but he’s alive. His kids are grown. He’s watching them graduate.
These aren’t outliers. They’re the people who listened.
Bottom Line
Alcoholic liver disease doesn’t happen overnight. It happens because you kept drinking when your body was screaming for you to stop. But every stage has a window. Fatty liver? Fixable. Alcoholic hepatitis? Treatable. Cirrhosis? Manageable-if you stop.
You don’t need to be an alcoholic to have alcohol-associated liver disease. You just need to drink too much, too often.
The liver is the most resilient organ in your body. But it has limits. And once those are crossed, there’s no going back.
But if you act now? You still have time.

The data presented here is both clinically rigorous and profoundly humanizing. The progression from steatosis to cirrhosis is not merely a medical trajectory-it is a narrative of bodily betrayal, often masked by social normalization. What stands out is the reversibility of early-stage damage, a fact too frequently overlooked in public discourse. The liver’s regenerative capacity, when given the chance, is one of medicine’s most elegant affirmations of biological resilience.
People think they’re just ‘having a few drinks’-but their liver’s screaming into a pillow while they post selfies with wine glasses. I’ve seen it. A woman I knew, 39, ‘social drinker,’ ended up in ICU with ascites. She thought she was in control. Turns out, her liver was already dead inside. No one warns you until your eyes turn yellow and your belly looks like you’re pregnant with a watermelon.
Let’s be real-this is just Big Pharma’s way of pushing sobriety as a product. Who says alcohol is the *real* villain? What about glyphosate in your beer? Or the corporate sugar lobby funding liver studies? They don’t want you to know the liver can detox *anything* if you just take the right supplements. The real cure? CBD oil, bentonite clay, and a 4 AM cold plunge. They’re burying this.
Thank you for writing this. 🌱 I lost my dad to cirrhosis. He never drank ‘hard’-just wine every night. He thought he was being ‘responsible.’ I wish someone had told him, gently, that ‘responsible’ doesn’t mean ‘safe’ when it’s daily. I’m sober now. Not because I was told to-but because I saw what silence does to a body. You’re not broken if you need help. You’re human.
They say alcohol causes liver damage. But what if it's the water? Or the plastic bottles? Or the government's hidden fluoride in beer? I read a paper-unpublished-linking liver fibrosis to 5G radiation exposure in urban bars. No one talks about it. The truth is buried.
While the article presents a clinically conventional narrative, it fails to interrogate the epistemological hegemony of Western hepatology. The concept of ‘reversibility’ in fatty liver is a reductionist construct, ignoring the biopolitical framing of addiction as a moral failure. The emphasis on abstinence as the sole intervention reflects a neoliberal pathology model-one that pathologizes pleasure while ignoring structural determinants like income inequality, labor alienation, and the commodification of leisure. One must ask: who benefits from the ‘sober narrative’? The pharmaceutical industry? The rehab-industrial complex? The answer lies not in liver enzymes-but in power.
Let me just say-I’ve been a nurse for 22 years, and I’ve seen this exact progression more times than I can count. You think you’re fine because you don’t get drunk? Wrong. You think you’re not an ‘alcoholic’ because you don’t drink in the morning? Wrong again. The liver doesn’t care about your labels. It only cares about volume, frequency, and duration. I had a patient-54, MBA, two kids, drinks two glasses of chardonnay every night since college-came in with stage 3 cirrhosis. No symptoms. No warning. Just a FibroScan and a death sentence. Stop rationalizing. Stop minimizing. Your liver isn’t a vending machine. It’s a life-support system. And it’s begging you to listen.
Isn’t it strange how we’ve turned a biological process into a moral crusade? The liver doesn’t judge. It metabolizes. It endures. It adapts. But we-humans-we assign guilt. Shame. Sin. We call it ‘alcoholic liver disease’ as if the alcohol is the villain, not the human behavior that glorifies its consumption. What if the real disease is our inability to sit with discomfort? To feel without numbing? To accept mortality without a bottle as a buffer? Maybe the cure isn’t sobriety… but presence. Maybe the liver isn’t the problem. Maybe we are.